



January 31, 2011
A study shows that a formulation of curcumin can relieve pain and increase mobility in patients with osteoarthritis. It can also reduce a series of inflammatory markers.
100 patients with osteoarthritis were divided in two groups -- the first group was given the "best available treatment" and the second group was given the same treatment plus 200 mg of the curcumin formulation each day.
According to IFT:
"The results showed that the [curcumin]-treated group had a statistically significant reduction in all primary clinical end-points ... These results were complemented by the evaluation of a series of inflammatory markers, soluble vascular cell adhesion molecule (sVCAM)-1, and erythrocyte sedimentation rate [ESR]) ... while no significant variation was observed in the 'best available treatment' group."
This could eventually lead to a phase out of NSAID use, at least as a treatment for mild-to-moderate osteoarthritis.
| Dr. Mercola's Comments: |
If you've never heard of curcumin -- the pigment that gives the curry spice turmeric its yellow-orange color -- you're in for a treat, as this is one natural compound that should be on your health radar. Curcumin is also the active ingredient in turmeric, which is a very popular supplement.
Both the ancient Chinese and Indian systems of medicine have recognized curcumin's beneficial properties for thousands of years, and now modern research is showing it may be one of nature's most powerful potential healers.
Most notably, curcumin is known for its potent anti-inflammatory properties. The compound has been shown to influence more than 700 genes, and it can inhibit both the activity and the synthesis of cyclooxygenase-2 (COX2) and 5-lipooxygenase (5-LOX), as well as other enzymes that have been implicated in inflammation.
One of the BEST Supplements for Many Cancers
Dr. William LaValley from Austin Texas, is one of the top natural medicine cancer physicians I know and he recently shared this important information on curcumin which has the most evidence based literature for as a cancer support among all nutrients. There are over 100 different pathways that curcumin has an effect on once it gets into the cell. Interestingly this also includes the metabolite of curcumin and its derivatives which are also anti-cancer. Curcumin appears to be safe in the treatment of all cancers.
In India where turmeric is widely used, the prevalence of four common U.S. cancers -- colon, breast, prostate and lung -- is 10 times lower. In fact, prostate cancer, which is the most frequently diagnosed cancer in U.S. men, is rare in India and this is attributed, in part, to the curcumin in turmeric.
Numerous studies have looked into this potential cancer-fighting link, with promising results. For instance, curcumin has been found to:
And according to researchers from the University of Texas M.D. Anderson Cancer Center, curcumin blocks a key biological pathway needed for development of melanoma and other cancers.
The spice actually stops laboratory strains of melanoma from proliferating and pushes the cancer cells to commit suicide by shutting down nuclear factor-kappa B (NF-kB), a powerful protein known to induce abnormal inflammatory response that leads to an assortment of disorders such as arthritis and cancer.
To get the full benefits that curcumin has to offer, you will want to look for a turmeric extract with at least 95% curcuminoids that contains only 100% certified organic ingredients.
The formula should be free of fillers, additives and excipients (a substance added to the supplement as a processing or stability aid), and the manufacturer should use safe production practices at all stages: planting, cultivation, selective harvesting, and then producing and packaging the final product.
Details on How to Use Curcumin
The unfortunate challenge as this time is that there are not really any very good formulations of curcumin available to use in cancer. This is because relatively high doses are required and curcumin is not absorbed that well. Typical anticancer doses are up to three grams of good bioavailable curcmin extract, three to four times daily.
One work around for this is to use the curcumin powder and make a microemulsion of it by combining a tablespoon of the powder and mixing it into 1-2 egg yolks and a teaspoon or two of melted coconut oil. Then using a high speed hand blender to emulsify the powder.
Another strategy you can use to increase absorption is to put one tablespoon of the curcumin powder into a quart of boiling water. It must be boiling when you add the powder as it will not work as well if you put it in room temperature water and heat the water and curcumin. After boiling it for ten minutes you will have created a 12% solution and you can drink this once it has cooled down. The curcumin will gradually fall out of solution over time and in about six hours it will be a 6% solution so it is best to drink the water within four hours. It does have a woody taste.
One caution to know is that you want to avoid the "yellow kitchen" syndrome. Curcumin is a very potent yellow pigment and can permanently discolor surfaces if you aren't careful. So you can perform the mixing under the hood of your stove with the blower on to make sure no powder gets into your kitchen.
Research Highlights Curcumin's Pain-Relieving Power
In the latest study of osteoarthritis patients, those who added 200 mg of curcumin a day to their treatment plan had reduced pain and increased mobility, whereas the control group, which received no curcumin, had no significant improvements.
A past study also found that a turmeric extract composed of curcuminoids (plant-based nutrients that contain powerful antioxidant properties) blocked inflammatory pathways, effectively preventing the launch of a protein that triggers swelling and pain.
A Natural Alternative to NSAIDs
Curcumin's anti-inflammatory effects help to reduce irritation to tissues characterized by pain, redness, swelling and heat, which is particularly helpful for osteoarthritis patients.
Osteoarthritis is a degenerative joint disease that causes joint stiffness, pain, inflammation and swelling that can become debilitating. Many patients turn to non-steroidal anti-inflammatories (NSAIDs) and analgesics, like Tylenol, for pain relief, but the regular, chronic use of these types of medications is associated with significant, and very serious, side effects such as cardiovascular problems, gastrointestinal harm and kidney and/or liver damage.
If you are taking an NSAID, you are at approximately three times greater risk for developing serious gastrointestinal side effects than those who aren't.
Approximately 1.2 percent of patients taking NSAIDs are actually hospitalized for upper GI problems, per year of exposure. One study of patients taking NSAIDs showed that a life-threatening complication was the first sign of ulcer in more than half of the subjects.
Researchers found that the drugs suppress production of prostacyclin, which is needed to dilate blood vessels and inhibit clotting. Earlier studies had found that mice genetically engineered to be unable to use prostacyclin properly were prone to clotting disorders.
Anyone who is at increased risk of cardiovascular disease should steer clear of these medications as well. Ulcer complications are certainly potentially life-threatening, but, heart attacks are a much more common and likely risk, especially in older individuals. So having a natural alternative to NSAIDs for pain relief is invaluable, especially for a painful condition like osteoarthritis.
You can use turmeric in your cooking (choose a pure turmeric powder, rather than a curry powder, as at least one study has found that curry powders tend to contain very little curcumin), but you may also want to consider taking it in supplement form.
For many this is a more convenient method to obtain the potential health benefits, especially if it is from a high-quality organic source, and also if you don't particularly enjoy the taste of curry. As an aside, curcumin is not only beneficial for osteoarthritis … research is also emerging showing it may play a beneficial role in the following diseases:
More Natural Tips for Osteoarthritis
Osteoarthritis, the deterioration of cartilage that cushions your joints, is the most common form of arthritis among the elderly. It's normally associated with "wear and tear" on your joints, but can also be caused by repetitive stress or acute trauma.
In addition to an anti-inflammatory like curcumin, I've long promoted omega-3 fats for arthritis because omega-3s are also well known to help reduce inflammation. Look for a high-quality, animal-based source such as krill oil. In addition, adding glucosamine to your omega-3s appears to be an excellent choice for osteoarthritis sufferers in particular.
If you have osteoarthritis, the cartilage within your joint is progressively being damaged, and the synovial fluid that keeps your joints lubricated and cushioned is typically reduced as well. The pain is a result of your bones starting to come into contact with each other as cartilage and synovial fluid is reduced.
Your body is fully capable of rebuilding cartilage and synovial fluid, but in order to effectively do so it needs the proper building blocks. In this case, it needs glucosamine to rebuild both cartilage and synovial fluid, so correcting this deficiency by using a high-quality supplement may be helpful.
In one study, participants with moderate-to-severe hip or knee osteoarthritis who received 1,500 mg of glucosamine sulfate along with 200 mg of omega-3 had greater pain reduction and fewer symptoms (morning stiffness, pain in hips and knees) than those who took glucosamine by itself.
I also recommend for osteoarthritis:
Your program should include a range of activities, just as I recommend for any exerciser. Weight training, cardio, stretching and core work can all be integrated into your routine, and, if your condition allows, it would be wise to move toward a Peak Fitness program that is designed for reaching optimal health.
There are several other natural strategies that can offer pain relief from osteoarthritis as well, including acupuncture, herbs like ginger and boswellia, bromelain and evening primrose oil.
By Dr. Mercola
 The war against illegal drug use has been going on for decades, but now it seems the “war on drugs” should have a new target… Legal drug addiction is taking lives in record numbers.
The war against illegal drug use has been going on for decades, but now it seems the “war on drugs” should have a new target… Legal drug addiction is taking lives in record numbers.
In the UK, 1 million people are addicted to over-the-counter (OTC) and prescription painkillers and tranquilizers; that’s significantly more than the number addicted to illegal drugs.1
In the US, it’s a similar story. There were four times more deaths among women from prescription painkiller overdose than for cocaine and heroin deaths combined in 2010.2
 Legal drug addiction is tricky because it often starts out with a prescription obtained from a doctor. Many people find themselves addicted to painkillers before they even realize what’s happened, often after taking the drugs to recover from surgery or treat chronic back, or other, pain.
Legal drug addiction is tricky because it often starts out with a prescription obtained from a doctor. Many people find themselves addicted to painkillers before they even realize what’s happened, often after taking the drugs to recover from surgery or treat chronic back, or other, pain.
Three Factors That Might Increase Your Risk of Becoming Addicted to Painkillers
Painkillers work by interacting with receptors in your brain resulting in a decrease in the perception of pain. They are inherently addictive, as they also create a temporary feeling of euphoria, followed by dysphoria, that can easily lead to physical dependence and addiction. However, why certain people become addicted while others get by unfazed has remained a mystery.
Researchers from the University of Derby set out to determine what might be influencing painkiller addiction and dependence by conducting an anonymous survey of people who had pain and had used painkillers in the last month. They found three predictors that they said identified those most at risk of developing painkiller dependence. It included those who:3
According to the authors, pain, prior substance abuse and psychological factors may all play a role in a person’s likelihood of addiction. They concluded:
“Based on these findings, a preliminary model is presented with three types of influence on the development of painkiller dependence: 1) pain leading to painkiller use, 2) risk factors for substance-related problems irrespective of pain, and 3) psychological factors related to pain.”
Painkiller Addiction Knows No Bounds
 The face of drug addiction in the US and around the globe is changing. You can certainly not gauge who is an addict by looks or occupation. In fact, painkiller addiction spans all ages and walks of life.
The face of drug addiction in the US and around the globe is changing. You can certainly not gauge who is an addict by looks or occupation. In fact, painkiller addiction spans all ages and walks of life.
For instance, a significant number of older adults, particularly those in the baby boomer generation, are struggling with both illicit and prescription drug abuse.
The National Institutes of Health (NIH) reported that the number of people in their 50s who are abusing illicit or prescription drugs more than doubled from 2002 to 2010, going from 2.7 to 5.8 percent in this population. Among those 65 and older, 414,000 used such drugs in 2010.4
Among seniors, the health risks of all medications are increased, because the body takes longer to break down and get rid of the drug than it does in a younger person. As a result, the drug stays in an older person's system longer, where it can cause even greater damage.
At the other end of the spectrum, one in four teens has misused a prescription drug at least once in their lifetime, according to survey results from the partnership at Drugfree.org and the MetLife Foundation.5 Prescription drugs don’t hold the same stigma as illegal recreational drugs, even though they can be just as deadly, leading teens to regard the former as a “safe” way to get high.
Prescription drugs have even been described by the White House Office of National Drug Control Policy as the “drug of choice” second only to marijuana for today’s teens.6
Sadly, some teens pay for this one “bad” decision with their lives. Drug fatalities more than doubled among teens and young adults between 2000 and 2008, and these drug-induced fatalities are not being driven by illegal street drugs. Data from the Centers for Disease Control and Prevention (CDC) found that the most commonly abused prescription drugs like OxyContin, Vicodin, Xanax, and Soma now cause more deaths than heroin and cocaine combined.7
And while men are still more likely to die from prescription painkiller overdose, women are quickly catching up. More than 6,600 women, or 18 women every day, died from a prescription painkiller overdose in 2010. The problem, once primarily seen in inner cities, is now spanning to rural areas, hitting people of all ethnic backgrounds and income levels, from business professionals to single mothers to retirees.
Painkiller Addiction Can Easily Lead to Death
Painkillers (opioids) like morphine, codeine, oxycodone, hydrocodone, and fentanyl are one of the most commonly abused drug classes. These drugs are not only addictive, they can lead to slowed breathing and death if too much is taken, and the risks are compounded if you add alcohol to the equation.
Many are not aware that pain-killing drugs like fentanyl are actually 100 times more potent than natural opioids like morphine, making the addictive potential and side effects associated with prescription drug use much higher. And it doesn’t always take extremely excessive use, or even very long-term use, to have a fatal overdose.
For many, once you start taking these drugs it sets off a cascade of reactions in your body that make it extremely difficult to stop. Dr. Sanjay Gupta, associate chief of neurosurgery at Grady Memorial Hospital and CNN's chief medical correspondent, reported:8
“…after just a few months of taking the pills, something starts to change in the body. The effectiveness wears off, and patients typically report getting only about 30% pain relief, compared with when they started. Even more concerning, a subgroup of these patients develop a condition known as hyperalgesia, an increased sensitivity to pain.
As you might guess, all of this creates a situation where the person starts to take more and more pills. And even though they are no longer providing much pain relief, they can still diminish the body's drive to breathe. If you are awake you may not notice it, but if you fall asleep with too many of these pills in your system, you never wake up. Add alcohol, and the problem is exponentially worse. People who take pain or sleeping pills and drink a couple glasses of wine are playing Russian roulette.”
 Because such overdoses now kill more people than cocaine and heroin combined, more US states are now taking action to try and stop this growing problem. As USA Today reported:9
Because such overdoses now kill more people than cocaine and heroin combined, more US states are now taking action to try and stop this growing problem. As USA Today reported:9
Managing Your Pain the Drug-Free Way
 Many of those addicted to painkillers started taking the drugs not to get high, but to control pain – often back pain. The solution, then, is to avoid taking the drugs in the first place, an option many physicians neglect to offer to their pain patients. If you are suffering from pain, I suggest you work with a knowledgeable health care practitioner to determine what's really triggering your pain, and then address the underlying cause. If you have chronic pain, try these first, before even thinking about prescription painkillers of any kind.
Many of those addicted to painkillers started taking the drugs not to get high, but to control pain – often back pain. The solution, then, is to avoid taking the drugs in the first place, an option many physicians neglect to offer to their pain patients. If you are suffering from pain, I suggest you work with a knowledgeable health care practitioner to determine what's really triggering your pain, and then address the underlying cause. If you have chronic pain, try these first, before even thinking about prescription painkillers of any kind.
It helps resolve underlying, often subconscious, negative emotions that may be exacerbating your physical pain. By stimulating (tapping) well-established acupuncture points with your fingertips, you rebalance your energy system, which tends to dissipate pain.
Courtesy of:
John H. Keefe III, D.C.
(918) 663-1111
Visit our web site: keefeclinic.com&facebook.com/keefeclinic
Belief not science is behind flu jab promotion, new
report says
BMJ2012;345 doi: http://dx.doi.org/10.1136/bmj.e7856
(Published 19 November 2012)
Cite this as:BMJ 2012; 345:e7856
Jeanne Lenzer
Author Affiliations
1New York An independent meta-analysis of vaccines against influenza has found that claims of benefit have been significantly exaggerated.
The report, released last month by the University of Minnesota’s Center for Infectious Disease Research and Policy, was based on a comprehensive review of data published from 1967 to 2012.
1Evidence for “consistent high-level protection is elusive,” the researchers concluded. Although vaccination was found to provide modest protection from infection in young healthy adults who rarely have complications of flu, the authors found that “evidence for protection in adults 65 years of age and older [who represent over 90% of deaths from flu] . . . is lacking.”
The authors also analyzed recommendations issued by the federal Advisory Committee on Immunization Practices, which provides expert advice to the US Centers for Disease Control and Prevention and which are “often considered the standard of practice . . .around the globe.” The report cited 30 instances in which its advisory statements “did not apply current standards of scientific rigor . . . and did not cite relevant work.”
The report’s lead author, Michael Osterholm, a former CDC consultant and an internationally recognized expert on flu, told the BMJ that a Dutch study cited by the CDC as evidence of vaccine efficacy was seriously flawed and constituted a “sales job.”
Nevertheless, Osterholm said, the current jab does offer some protection and should be used until a more effective vaccine can be developed.
Joseph Bresee, chief of the epidemiology and prevention branch in CDC’s Influenza Division, told the BMJ , “I do not agree that CDC has inflated the benefits of influenza vaccine.” He added that he agreed with Osterholm that until better vaccines were available the current ones should be recommended.
That recommendation, however, has come under fire from the authors of a Cochrane analysis that also found little to no benefit from flu vaccination.2 Tom Jefferson, lead author of several Cochrane reviews, told the BMJ, “Based on more than a decade of Cochrane reviews in adults, children, [the] elderly, and healthcare workers, there is no credible evidence that the inactivated vaccines have any effect other than saving on average half a working day in healthy adults and avoiding symptoms in those who least need it: healthy adults and adolescents. Depending on the season, you need to immunize 33 to 99 adults to avoid one set of symptoms.”
Osterholm criticized the methods of the Cochrane analysis, saying that the reviewers’ inclusion of studies that used serology titers rather than reverse transcription polymerase chain reaction or cultures to diagnose flu meant that its results were highly inaccurate.
However, he acknowledged that the direction of bias caused by use of serology titers would be to make a vaccine seem far more effective than it was, a surprising bias for a meta-analysis that found no benefit for flu vaccines. The Cochrane reviewers also stated in their meta-analysis that the studies reviewed were “at high risk of bias.”
A growing number of healthcare facilities and states now require healthcare workers to be vaccinated against flu or face being fired or forced to wear masks and identification tags stating that they may be infectious.
A recent editorial in the journal of the Canadian Medical Association,CMAJ, recommending mandatory flu jabs for healthcare staff triggered strong criticism, including a letter to the editor from Peter Doshi, a postdoctoral fellow at Johns Hopkins University, and several Cochrane reviewers, who said that the recommendation was based on a misrepresentation of Cochrane data.
34 Doshi opposes compulsory vaccination. He told the BMJ that health officials “risk losing credibility by continuing to promote the fiction that mandatory influenza vaccination policies are based on solid evidence. They are not, and it is time for healthcare institutions to do their own rigorous assessment of the evidence rather than continuing this dangerous game of follow the leader.” Osterholm agreed that scientific evidence, not professional opinions, should guide policy. He told the BMJ , “I don’t think the data warrant mandated vaccine. If it was up to me, there are a hundred other things I’d mandate first, like mandating that sick healthcare workers don’t come to work. That is far more likely to be effective.”
Notes:Cite this as: BMJ 2012;345:e7856
Footnotes
bmj.com
News: Bias alone could account for benefit attributed to flu vaccine, study finds (2008;337:a1550, doi:10.1136/bmj.a1550); Observations: A jab in the dark (2012;345:e5313, doi:10.1136/bmj.e5313)
References
1.Osterholm MT, Kelly NS, Manske JM, Ballering KS, Leighton TR, Moore KA. The compelling need for game-changing influenza vaccines: an analysis of the influenza vaccine enterprise and recommendations for the future. University of Minnesota Center for Infectious Disease Research and Policy, Oct 2012. www.cidrap.umn.edu/cidrap/center/mission/articles/ccivi-landing.html
.
Courtesy of:
John H. Keefe III, D.C.
(918) 663-1111
IN THE NEWS: SIDE EFFECTS FROM ADHD DRUGS MAY BE WORSE THAN ADHD The side effects from ADHD medications are often far worse than the condition itself. These drugs actually rival illegal street drugs in terms of their dangerous risks to health, which include: Permanent brain damage, Cardio toxicity and liver damage, Cancer, Changes in personality, depression, and/or hallucinations, Heart attack and stroke, Sudden death and suicide. This is a more than 400 percent increase in ER visits due to adverse reactions to such drugs in a mere six years! Drugs prescribed for ADHD are not "mild" by any means. These are hard-core, "class 2" narcotics, regulated by the Drug Enforcement Agency as a controlled substance because they can lead to dependence. The majority of kids diagnosed with ADHD will be prescribed these potentially dangerous drugs, the most common being Ritalin. By definition, Ritalin stimulates your central nervous system and may certainly interfere with the delicate and complex workings of your brain and personality.
WELLNESS: SLEEP HELPS DETOX THE BRAIN We’ve known for some time that sleep is essential for forming and consolidating memories and that it plays a central role in the formation of new neuronal connections and the pruning of old ones. But that hardly seems enough to risk death-by-leopard-in-the-night. “If sleep was just to remember what you did yesterday, that wouldn’t be important enough,” Dr. Nedergaard explains. In a series of new studies, published this fall in the journal Science, the Nedergaard lab may at last be shedding light on just what it is that would be important enough. Sleep, it turns out, may play a crucial role in our brain’s physiological maintenance. As your body sleeps, your brain is quite actively playing the part of mental janitor: It’s clearing out all of the junk that has accumulated as a result of your daily thinking. In a series of new studies on mice, her team discovered exactly that: When the mouse brain is sleeping or under anesthesia, it’s busy cleaning out the waste that accumulated while it was awake. On average, we’re getting one to two hours less sleep a night than we did 50 to 100 years ago and 38 minutes less on weeknights than we did as little as 10 years ago. At the extreme end, the result could be the acceleration of neurodegenerative diseases like Alzheimer’s and Parkinson’s.
CHIROPRACTIC: ADJUSTMENTS HAVE A POSITIVE EFFECT ON THE BRAIN A study presented at the International Research And Philosophy Symposium held at Sherman College of Straight Chiropractic finds that Chiropractic adjustments have a positive effect on the Central Nervous System (CNS), specifically on the four primary frequencies of brain function. Brain function is measured on four primary frequencies: Beta, Alpha, Theta and Delta. Alpha waves reflect the meditative, relaxing healing mode. Beta waves represent the active, busy brain. Theta waves reflect light sleep, relaxation and conceptual development. Delta waves represent the brain activity during deep sleep, repair mode and energy storage. After receiving a chiropractic adjustment, post EEG scans revealed improvement in all areas of the volunteer’s brain function. Particularly, the researchers noticed an increase in the meditative Alpha brainwave patterns that are associated with a greater degree of relaxation, health and healing. Visit our web site: keefeclinic.com or facebook/keefeclinic.com
SLEEP seems like a perfectly fine waste of time. Why would our bodies evolve to spend close to one-third of our lives completely out of it, when we could instead be doing something useful or exciting? Something that would, as an added bonus, be less likely to get us killed back when we were sleeping on the savanna?
“Sleep is such a dangerous thing to do, when you’re out in the wild,” Maiken Nedergaard, a Danish biologist who has been leading research into sleep function at the University of Rochester’s medical school, told me. “It has to have a basic evolutional function. Otherwise it would have been eliminated.”
We’ve known for some time that sleep is essential for forming and consolidating memories and that it plays a central role in the formation of new neuronal connections and the pruning of old ones. But that hardly seems enough to risk death-by-leopard-in-the-night. “If sleep was just to remember what you did yesterday, that wouldn’t be important enough,” Dr. Nedergaard explains.
In a series of new studies, published this fall in the journal Science, the Nedergaard lab may at last be shedding light on just what it is that would be important enough. Sleep, it turns out, may play a crucial role in our brain’s physiological maintenance. As your body sleeps, your brain is quite actively playing the part of mental janitor: It’s clearing out all of the junk that has accumulated as a result of your daily thinking.
Recall what happens to your body during exercise. You start off full of energy, but soon enough your breathing turns uneven, your muscles tire, and your stamina runs its course. What’s happening internally is that your body isn’t able to deliver oxygen quickly enough to each muscle that needs it and instead creates needed energy anaerobically. And while that process allows you to keep on going, a side effect is the accumulation of toxic byproducts in your muscle cells. Those byproducts are cleared out by the body’s lymphatic system, allowing you to resume normal function without any permanent damage.
The lymphatic system serves as the body’s custodian: Whenever waste is formed, it sweeps it clean. The brain, however, is outside its reach — despite the fact that your brain uses up about 20 percent of your body’s energy. How, then, does its waste — like beta-amyloid, a protein associated with Alzheimer’s disease — get cleared? What happens to all the wrappers and leftovers that litter the room after any mental workout?
“Think about a fish tank,” says Dr. Nedergaard. “If you have a tank and no filter, the fish will eventually die. So, how do the brain cells get rid of their waste? Where is their filter?”
UNTIL a few years ago, the prevailing model was based on recycling: The brain got rid of its own waste, not only beta-amyloid but other metabolites, by breaking it down and recycling it at an individual cell level. When that process eventually failed, the buildup would result in age-related cognitive decline and diseases like Alzheimer’s. That “didn’t make sense” to Dr. Nedergaard, who says that “the brain is too busy to recycle” all of its energy. Instead, she proposed a brain equivalent of the lymphatic system, a network of channels that cleared out toxins with watery cerebrospinal fluid. She called it the glymphatic system, a nod to its dependence on glial cells (the supportive cells in the brain that work largely to maintain homeostasis and protect neurons) and its function as a sort of parallel lymphatic system.
She was hardly the first to think in those terms. “It had been proposed about one hundred years ago, but they didn’t have the tools to study it properly,” she says. Now, however, with advanced microscopes and dyeing techniques, her team discovered that the brain’s interstitial space — the fluid-filled area between tissue cells that takes up about 20 percent of the brain’s total volume — was mainly dedicated to physically removing the cells’ daily waste.
When members of Dr. Nedergaard’s team injected small fluorescent tracers into the cerebrospinal fluid of anesthetized mice, they found that the tracers quickly entered the brain — and, eventually, exited it — via specific, predictable routes.
The next step was to see how and when, exactly, the glymphatic system did its work. “We thought this cleaning process would require tremendous energy,” Dr. Nedergaard says. “And so we asked, maybe this is something we do when we’re sleeping, when the brain is really not processing information.”
In a series of new studies on mice, her team discovered exactly that: When the mouse brain is sleeping or under anesthesia, it’s busy cleaning out the waste that accumulated while it was awake.
In a mouse brain, the interstitial space takes up less room than it does in ours, approximately 14 percent of the total volume. Dr. Nedergaard found that when the mice slept, it swelled to over 20 percent. As a result, the cerebrospinal fluid could not only flow more freely but it could also reach further into the brain. In an awake brain, it would flow only along the brain’s surface. Indeed, the awake flow was a mere 5 percent of the sleep flow. In a sleeping brain, waste was being cleared two times faster. “We saw almost no inflow of cerebrospinal fluid into the brain when the mice were awake, but then when we anesthetized them, it started flowing. It’s such a big difference I kept being afraid something was wrong,” says Dr. Nedergaard.
Similar work in humans is still in the future. Dr. Nedergaard is currently awaiting board approval to begin the equivalent study in adult brains in collaboration with the anesthesiologist Helene Benveniste at Stony Brook University.
So far the glymphatic system has been identified as the neural housekeeper in baboons, dogs and goats. “If anything,” Dr. Nedergaard says, “it’s more needed in a bigger brain.”
MODERN society is increasingly ill equipped to provide our brains with the requisite cleaning time. The figures are stark. Some 80 percent of working adults suffer to some extent from sleep deprivation. According to the National Sleep Foundation, adults should sleep seven to nine hours. On average, we’re getting one to two hours less sleep a night than we did 50 to 100 years ago and 38 minutes less on weeknights than we did as little as 10 years ago. Between 50 and 70 million people in the United States suffer from some form of chronic sleep disorder. When our sleep is disturbed, whatever the cause, our cleaning system breaks down. At the University of Pennsylvania’s Center for Sleep and Circadian Neurobiology, Sigrid Veasey has been focusing on precisely how restless nights disturb the brain’s normal metabolism. What happens to our cognitive function when the trash piles up?
At the extreme end, the result could be the acceleration of neurodegenerative diseases like Alzheimer’s and Parkinson’s. While we don’t know whether sleep loss causes the disease, or the disease itself leads to sleep loss — what Dr. Veasey calls a “classic chicken-and-egg” problem — we do know that the two are closely connected. Along with the sleep disturbances that characterize neurodegenerative diseases, there is a buildup of the types of proteins that the glymphatic system normally clears out during regular sleep, like beta-amyloids and tau, both associated with Alzheimer’s and other types of dementia.
“To me,” says Dr. Veasey, “that’s the most compelling part of the Nedergaard research. That the clearance for these is dramatically reduced from prolonged wakefulness.” If we don’t sleep well, we may be allowing the very things that cause neural degeneration to pile up unchecked.
Even at the relatively more benign end — the all-nighter or the extra-stressful week when you caught only a few hours a night — sleep deprivation, as everyone who has experienced it knows, impedes our ability to concentrate, to pay attention to our environment and to analyze information creatively. “When we’re sleep-deprived, we can’t integrate or put together facts,” as Dr. Veasey puts it.
But there is a difference between the kind of fleeting sleep loss we sometimes experience and the chronic deprivation that comes from shift work, insomnia and the like. In one set of studies, soon to be published in The Journal of Neuroscience, the Veasey lab found that while our brains can recover quite readily from short-term sleep loss, chronic prolonged wakefulness and sleep disruption stresses the brain’s metabolism. The result is the degeneration of key neurons involved in alertness and proper cortical function and a buildup of proteins associated with aging and neural degeneration.
It’s like the difference between a snowstorm’s disrupting a single day of trash pickup and a prolonged strike. No longer quite as easy to fix, and even when the strike is over, there’s likely to be some stray debris floating around for quite some time yet. “Recovery from sleep loss is slower than we’d thought,” Dr. Veasey notes. “We used to think that after a bit of recovery sleep, you should be fine. But this work shows you’re not.”
If you put her own research together with the findings from the Nedergaard lab, Dr. Veasey says, it “very clearly shows that there’s impaired clearance in the awake brain. We’re really starting to realize that when we skip sleep, we may be doing irreparable damage to the brain, prematurely aging it or setting it up for heightened vulnerability to other insults.”
In a society that is not only chronically sleep-deprived but also rapidly aging, that’s bad news. “It’s unlikely that poor sleep as a child would actually cause Alzheimer’s or Parkinson’s,” says Dr. Veasey, “but it’s more likely that you may shift one of those diseases by a decade or so. That has profound health and economic implications.”
It’s a pernicious cycle. We work longer hours, become more stressed, sleep less, impair our brain’s ability to clean up after all that hard work, and become even less able to sleep soundly. And if we reach for a sleeping pill to help us along? While work on the effects of sleeping aids on the glymphatic system remains to be done, the sleep researchers I spoke with agree that there’s no evidence that aided sleep is as effective as natural sleep.
There is, however, reason to hope. If the main function of sleep is to take out our neural trash, that insight could eventually enable a new understanding of both neurodegenerative diseases and regular, age-related cognitive decline. By developing a diagnostic test to measure how well the glymphatic system functions, we could move one step closer to predicting someone’s risk of developing conditions like Alzheimer’s or other forms of dementia: The faster the fluids clear the decks, the more effectively the brain’s metabolism is functioning.
“Such a test could also be used in the emergency room after traumatic brain injury,” Dr. Nedergaard says, “to see who is at risk of developing decline in cognitive function.”
We can also focus on developing earlier, more effective interventions to prevent cognitive decline. One approach would be to enable individuals who suffer from sleep loss to sleep more soundly — but how? Dr. Nedergaard’s mice were able to clear their brain’s waste almost as effectively under anesthesia as under normal sleeping conditions. “That’s really fascinating,” says Dr. Veasey. Though current sleeping aids may not quite do the trick, and anesthetics are too dangerous for daily use, the results suggest that there may be better ways of improving sleep pharmacologically.
Now that we have a better understanding of why sleep is so important, a new generation of drug makers can work to create the best possible environment for the trash pickup to occur in the first place — to make certain that our brain’s sleeping metabolism is as efficient as it can possibly be.
A second approach would take the opposite tack, by seeking to mimic the cleanup-promoting actions of sleep in the awake brain, which could make a full night of sound sleep less necessary. To date, the brain’s metabolic process hasn’t been targeted as such by the pharmaceutical industry. There simply wasn’t enough evidence of its importance. In response to the evolving data, however, future drug interventions could focus directly on the glymphatic system, to promote the enhanced cleaning power of the sleeping brain in a brain that is fully awake. One day, scientists might be able to successfully mimic the expansion of the interstitial space that does the mental janitorial work so that we can achieve maximally efficient round-the-clock brain trash pickup.
If that day comes, they would be on their way to discovering that all-time miracle drug: one that, in Dr. Veasey’s joking words, “could mean we never have to sleep at all.”
MORE ON SLEEP
http://www.keefeclinic.com/wp/20-ways-to-sleep-better-every-night/
Alan Cassels, MD, states on the first page of his recent book, Seeking Sickness: How the World’s Biggest Pharmaceutical Companies Are Turning Us All into Patients, “Medical screening is a powerful, seductive and highly intuitive thing to do … However, much of what passes for prevention—with medical screening as its centerpiece—is expensive, often misguided, and frequently counterproductive.”
How can this be? After all, we’ve been hearing for years, and sometimes found ourselves repeating, that it’s always better to know what’s happening, that finding abnormalities early is always best, and that the benefits of screenings outweigh their harms. Are we now being asked to accept that these pearls of consensus wisdom are wholly or largely incorrect? And if so, how could we all have been led down this path?
Screenings Primarily Identify Mild Cases or Those with Risk Factors Only
As Gilbert Welch, a primary care physician at a Vermont Veterans Administration hospital and Professor of Medicine at the Dartmouth Institute for Health Policy and Clinical Practice, writes in his equally powerful book, Overdiagnosed: Making People Sick in Pursuit of Health, the problem with screening is that it inevitably identifies as candidates for further diagnosis and therapy many individuals who have mild versions of a condition, along with those who do not have the condition at all and may never manifest it, but are found to have risk factors for the disease in question.
These two categories (mild illness and risk factors in the absence of illness) now constitute the majority of those identified by screening, who are the people least likely to benefit from medical treatment, and thus most likely to have a negative risk-benefit ratio. For many of us who have long advocated strongly for prevention, and who have seen screenings as a key part of disease prevention and health promotion strategies, it may be time to rethink our views.
I have been an enthusiastic proponent of preventive services, including screenings related to heart disease, cancer, diabetes, hypertension, and the other major chronic degenerative diseases of our time. This was a key topic in my most widely disseminated article1 and also was addressed in two later peer-reviewed articles I co-authored.2,3 Moreover, during the years I was involved in direct patient care, and at the institution where I now teach, I have encouraged these screening procedures and taught students to value them. I have seen the information gleaned from screenings as a tool to enable patients to know more about their own health, in the hope that this will guide them toward health-affirming behaviors.
Because we live in a time and place where the major killers are chronic degenerative diseases rather than infectious diseases, it seems logical to find out who is most susceptible to these ailments and then to provide lifestyle-based preventive counseling to fend off their onset for as long as possible. Such an approach is of great value, but primary prevention is increasingly being defined more in terms of early detection of disease and risk factors, and less in terms of the deeper level of prevention found in lifestyle-based counseling. Based on accelerating trends elucidated in four books4-7 by physician-authors that I have recently read, I am growing increasingly worried that screening efforts, however well-intentioned, may serve as an entrenched pipeline for lifelong pharmaceutical therapies that often are not needed and in many cases are harmful. I am still coming to terms with this shift in my perspective.
Is the Prevention Movement Being Hijacked?
I am deeply concerned that prevention, which is very desirable conceptually, is being hijacked for purposes that do not serve public health well. The question is: do mass screenings do more good than harm?
There is no question that screenings help some individuals and save some lives. But how many people are harmed in the process? To flesh this out with real world examples (based on Cassels’ and Welch’s writings), we need to ask the following: (1) how many people will be harmed by false positive or false negative diagnoses? and (2) how many people will need to be treated for many years with, for example, medication for hypertension or osteoporosis, in order to prevent one death, one stroke or one hip fracture? Without those answers, we are flailing in the dark.
Ethical Arguments Pro and Con
The argument in favor of widespread screening is quite straightforward. If we can determine which people in a population are at risk for certain diseases or already have those diseases, as long as effective treatments exist we can deliver those treatments and presumably serve their welfare. Thus, there exists an ethical foundation for population screening as a first step toward further testing of those whose screenings reveal risk factors and subsequent treatment of those found to have frank expression of disease. But the foundation used to justify widespread population screenings rests entirely on whether the benefits outweigh the harms. Absent that, widespread screening is unethical.
The argument against widespread screening programs is that they cast far too wide a net, ensnaring people who are largely healthy, labeling them permanently as patients, subjecting them to a range of invasive diagnostic and therapeutic procedures (including drug therapies), and in the process causing many people both physical and psychological harm. As Dr. Welch puts it in Overdiagnosed, “We are in the midst of an epidemic of overdiagnosis … Diagnosis is a double-edged sword. While it has the potential to help some, it always has a hidden danger: overdiagnosis—the detection of abnormalities that are not destined to ever bother us.”
Screenings and Overdiagnosis
Contrary to widespread and deeply-ingrained belief, more diagnosis and earlier diagnosis does not necessarily mean better health care. It does mean more treatment, but more treatment brings more negative side effects. If a dangerous condition is mitigated or cured in the process, this may be a reasonable trade-off. But when people with mild versions of conditions such as hypertension, cardiovascular disease, or prostate cancer, or risk factors in the absence of such diseases, undergo invasive diagnostic and therapeutic procedures, or are placed on life-long drug prescriptions, the trade-off may be a losing proposition. This is particularly true in cases where only risk factors for disease, rather than disease itself, are identified through screening.
Further complicating the issue, in recent years medical guidelines regarding which patients should be placed on drug therapy (statins for heart disease are Exhibit A) have been repeatedly ratcheted down, by committees with strong ties to drug manufacturers. In late 2013, this reached the point where, as noted in a recent New York Times article, “Dr. Nissen [of Cleveland Clinic in Ohio] entered the figures for a 60-year-old African-American man with no risk factors — total cholesterol of 150, HDL (the good cholesterol) of 45, systolic blood pressure of 125 — who was not a diabetic or a smoker. He ended up with a 10-year risk of 7.5 percent, meaning he should be taking cholesterol-lowering statins despite being in a seemingly low-risk group. Dr. Nissen also calculated the figures for a healthy white man, age 60, and also got a risk factor of 7.5 percent.”
Again, we return to the key question: are we doing more harm than good?
In the case of typical medical, chiropractic, or other practitioners recommending or requiring screenings of all patients for a wide range of conditions, I think we should assume that this is done with the best of intentions. And if there is a serious, sustained effort to pursue diet and exercise-based approaches as the first-line approach, I certainly see screenings as a net positive. But after reading these books by Cassels, Welch and others, along with many related articles8-13 for a public health ethics class I just completed, it is clear to me that no such assumption of public-spirited service should ever be granted to pharmaceutical companies, who provide hundreds of millions of dollars to overtly and covertly support widespread screenings and guidelines that encourage vast increases in drug use. These companies also routinely hide the results of the clinical trials they fund that have determined their drugs to be ineffective or harmful. In some cases, these very drugs yield profits measured in billions of dollars.
For an excellent discussion of current trends on prevention and wellness in chiropractic education and practice, I recommend an excellent 2013 article14 (full text here) by Drs. Cheryl Hawk and Will Evans in Chiropractic and Manual Therapies, as well as their book, Health Promotion and Wellness: An Evidence-Based Guide to Clinical Preventive Services (Lippincott Williams and Wilkins, 2013).15 [Disclosure: I wrote the nutrition chapter in this book.] Because chiropractors recognize the importance of lifestyle-based counseling as the first-line approach, and also recognize the need for medical therapies in more serious cases, the Hawk-Evans approach to clinical preventive services illustrates what I believe is the best available way forward. Needless to say, these two DC-PhD authors are free of drug company conflicts of interest.
Let’s close with an excerpt (Selling Sickness, p. 121) from Dr. Cassels’ chapter on the history of selling osteoporosis drugs, the bisphosphenates such as Fosamax:
“Prior to September 29, 1995, when the U.S. FDA approved Fosamax for the treatment of osteoporosis, that disease was largely unknown to the general public or even to medicine. To understand how we got from there to here is to understand the issue of surrogacy. Intermediate, or surrogate, markers—such as blood pressure, body-mass index, cholesterol levels, intraocular pressure, or, in the case of osteoporosis, bone-mineral density readings—are markers for disease. Your high cholesterol or blood pressure may not be obvious to you, but you don’t want to have a heart attack. In the case of osteoporosis, the reading of your T-score isn’t as important as whether you fracture.
“Many women with low T-scores will never have a fracture in their lives, and many women with ‘normal’ bone density will have fractures. But the point is that a T-score can be measured, assigned a value, and a drug can be given to try to alter that measurement. The goal then, for those with a drug to sell, is to sell the testing first, because without the test you’d have no market. A number of PR firms working in the field of osteoporosis in the mid-1990s were key in reconfiguring osteoporosis from a rare disease that was believed only to strike old ladies to something anyone of any age could get. And in the shadows, funding these activities were pharmaceutical companies like Merck, banking on a big market for its new drug Fosamax.
“The strategy was simple: First, convince women at younger and younger ages that they needed to be screened for this bone-weakening disease, so they were urged through ads and so on to consult their doctors for a bone-density test. Second, the bone- density testing machines needed to be in physicians’ offices, private clinics, and hospitals, so the manufacturers bought and distributed the machines. Third, the tests needed to be paid for, so the PR firms needed to lobby governments to cover the bone-density test. What most people don’t know is that if you define a disease broadly enough, you can capture a large part of the ‘healthy’ population.
“Most also won’t know that drug company executives found themselves at the table at a meeting of the World Health Organization in 1995, helping to create the very definition of osteoporosis. The definition they created was so broad—based on the arbitrary value of the T-score—that it meant that about 50 percent of post-menopausal women in the United States (or about 44 million women) had it. And the message that flowed from the popular press strongly suggested that even the healthiest people should be worried about falling and breaking a hip due to the weakening of their bones.”
The hijacking of prevention continues, with much more than can be contained in this book review. The key take-home message is that for numerous conditions, drugs that may be helpful for a relatively small number of people are being pushed by multinational pharmaceutical companies as appropriate, indeed necessary, for large portions of the population, without evidence that this will do more good than harm. The downside usually becomes known years after millions have taken the drugs, sometimes with disastrous effects.
It is heartening that physician-authors are writing books to make these stories better known. What is needed now is for books like these be read widely, for more people to ask questions, and for policy makers and regulators to do a far better job of protecting the public from predatory drug companies.
References
1. Redwood D. The health reform moment: peril and possibility in the Obama era. J Altern Complement Med. Jan 2009;15(1):1-3.
2. Globe G, Redwood D, Brantingham JW, et al. Improving preventive health services training in chiropractic colleges part II: enhancing outcomes through improved training and accountability processes. J Manipulative Physiol Ther. Jul-Aug 2009;32(6):453-462.
3. Hawk C, Schneider M, Evans MW, Jr., Redwood D. Consensus process to develop a best-practice document on the role of chiropractic care in health promotion, disease prevention, and wellness. J Manipulative Physiol Ther. Sep 2012;35(7):556-567.
4. Welch G, Schwartz L, Woloshin S. Overdiagnosed: Making People Sick in Pursuit of Health. Boston. Beacon Press. 2011.
5. Moynihan R, Cassels A. Selling Sickness: How the World’s Biggest Pharmaceutical Companies Are Turning Us All into Patients. Vancouver/Toronto/Berkeley. Greystone Books. 2005.
6. Cassels A. Seeking Sickness: Medical Screening and the Misguided Hunt for Disease. Vancouver/Toronto/Berkeley. Greystone Books. 2011.
7. Hadler N. Rethinking Aging: Growing Old and Living Well in an Overtreated Society. Chapel Hill. University of North Carolina Press. 2011.
8. Fletcher SW. Breast Cancer Screening: A 35-Year Perspective. Epidemiologic Reviews. July 1, 2011 2011;33(1):165-175.
9. Foster P, Anderson, CM. Reaching targets in the national cervical screening programme: are current practices unethical? Journal of Medical Ethics. 1998;24:151-157.
10. Rychetnik L, Carter SM, Abelson J, et al. Enhancing citizen engagement in cancer screening through deliberative democracy. J Natl Cancer Inst. Mar 20 2013;105(6):380-386.
11. Shickle D, Chadwick R. The ethics of screening: is 'screeningitis' an incurable disease? J Med Ethics. Mar 1994;20(1):12-18.
12. Skrabanek P. Why is preventive medicine exempted from ethical constraints? J Med Ethics. Dec 1990;16(4):187-190
13. Takala T, Gylling HA. Who Should Know about Our Genetic Makeup and Why? J Med Ethics. 2000;26(3):171-174
14. Hawk C, Evans MW, Jr. A framework for chiropractic training in clinical preventive services. Chiropr Man Therap. 2013;21(1):28.
15. Hawk C, Evans MW. Health Promotion and Wellness: An Evidence-Based Guide to Clinical Preventive Services Philadelphia: Lippincott Williams and Wilkins; 2013.
Daniel Redwood, DC, is a Professor at Cleveland Chiropractic College – Kansas City. He is the Editor-in-Chief of Health Insights Today, Associate Editor of Topics in Integrative Healthcare and serves on the editorial board of the American Chiropractic Association. Dr. Redwood’s website and health policy blog are at www.redwoodhealthspeak.com.
Courtesy of:
John H. Keefe III, D.C.
(918) 663-1111
DIET: HOW LEPTIN RESISTANCE CAUSES OBESITY In order for you to significantly gain weight, you must first become leptin resistant. Leptin is a hormone that helps you regulate your appetite. When your leptin levels rise, it signals your body that you’re full, so you’ll stop eating. However, as you become increasingly resistant to the effects of leptin, you end up eating more. Many people who are overweight also have an impairment in their body’s ability to oxidize fat, which leads to a low-energy state. The question then is: what drives this basic process? Why do you become leptin resistant in the first place? Research clearly shows that refined sugar (in particular fructose) is exceptionally effective at causing leptin resistance in animals, and it’s very effective at blocking the burning of fat. When you give fructose to animals, they lose their ability to control their appetite, they eat more, and they exercise less. Fructose looks like it’s playing a direct role in weight gain.
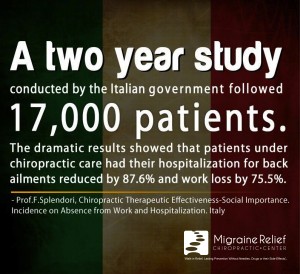
CHIROPRACTIC: DID YOU KNOW A 2009 evidence-based report on population, health and total health care spending suggested that chiropractic care of back pain and neck pain provides higher satisfaction, superior outcomes and more cost-effectiveness than other commonly-utilized back and neck pain treatments, which can include simple rest, medications, surgery and more. A further review of scientific literature indicated that patients with chiropractic coverage as part of their insurance benefits had lower costs and reduced imaging studies, fewer hospitalizations and less surgeries than patients without chiropractic included in their insurance. Based upon a friend's referral, I started chiropractic care for my migraine headaches. I have learned that the spine controls the nerves, when a nerve is pinched or moved it can cause pain. I no longer have headaches or constant back pain. After the adjustments, my headaches are better. -Linda
Visit our web site: keefeclinic.com&facebook.com/keefeclinic
Received 4 May 2013; received in revised form 25 July 2013; accepted 1 August 2013. published online 21 November 2013.
Abstract
Objective
The purpose of this study was to develop evidence-based treatment recommendations for the treatment of nonspecific (mechanical) neck pain in adults.
Methods
Systematic literature searches of controlled clinical trials published through December 2011 relevant to chiropractic practice were conducted using the databases MEDLINE, EMBASE, EMCARE, Index to Chiropractic Literature, and the Cochrane Library. The number, quality, and consistency of findings were considered to assign an overall strength of evidence (strong, moderate, weak, or conflicting) and to formulate treatment recommendations.
Results
Forty-one randomized controlled trials meeting the inclusion criteria and scoring a low risk of bias were used to develop 11 treatment recommendations. Strong recommendations were made for the treatment of chronic neck pain with manipulation, manual therapy, and exercise in combination with other modalities. Strong recommendations were also made for the treatment of chronic neck pain with stretching, strengthening, and endurance exercises alone. Moderate recommendations were made for the treatment of acute neck pain with manipulation and mobilization in combination with other modalities. Moderate recommendations were made for the treatment of chronic neck pain with mobilization as well as massage in combination with other therapies. A weak recommendation was made for the treatment of acute neck pain with exercise alone and the treatment of chronic neck pain with manipulation alone. Thoracic manipulation and trigger point therapy could not be recommended for the treatment of acute neck pain. Transcutaneous nerve stimulation, thoracic manipulation, laser, and traction could not be recommended for the treatment of chronic neck pain.
Conclusions
Interventions commonly used in chiropractic care improve outcomes for the treatment of acute and chronic neck pain. Increased benefit has been shown in several instances where a multimodal approach to neck pain has been used.
This article is a rebuttal to the recently publicized negative study offish oil and prostate cancer compiled by a panel of Nutri- West experts: Lynn Toohey, PhD; Don Bellgrau PhD (NIH grant reviewer); Dan Murphy D, DABCO (years of research on omega 3s; part time faculty, Life Chiropractic College West), Brandon Lundell, DC, DABCI instructor, Assistant Professor, So. Cal. U of Health Sciences.
In a word: fiction. Recently, headlines touted a negative association of fish oil and prostate cancer (Brasky et al. 2013)', based on an observational study (not a clinical trial proving cause and effect) that analyzed (after the fact) previous data taken from a publication that did not adjust for what they call confounding factors - other factors that can cause prostate cancer The conclusions that they drew from their observations have been rebutted by experts in the field, and called everything from "silly" to "irresponsible". An association was not only mistakenly drawn, it was given wide media coverage, mostly because it goes against everything we have been told is true (based on good research) that fish oil is good for us. This misinterpretation of facts certainly does not negate all of the thousands of positive articles on fish oil, which include well-designed, randomized placebo controlled CLINICAL TRIALS, in which participants are actually given fish oil and then results are measured.
The Science of Interpreting Studies: It is taught in every first year doctorate program that when you read a study, in order to avoid drawing false conclusions, one must remember the axiom: Correlation Does Not Imply Causation. In this study, the flawed correlation of prostate cancer with Omega 3's in the blood does not in any way mean that Omega 3's cause prostate cancer. Even if a correlation did exist (which is unlikely as you will see below) the Omega 3's could be elevated because of the cancer and not the other way around. Cancer is known to alter metabolism in various ways, including fatty acid metabolism. It is more conceivable, given the preponderance of evidence of beneficial effects of Omega 3's, that cancer induces inflammatory chemicals which in turn release fatty acids into the blood stream. This could be a host —defense mechanism, or a tactic on part of the cancer cells to supply ample energy for tumorigenesis. In any case, one must remember the axiom "correlation does not imply causation".
This study in question was riddled with many flaws, including the fact that they did not measure fish oil intake, or even fish oil supplements for that matter (and we all know that there is a difference between farm raised fish and wild caught salmon!) What they measured was the level of fatty acids in the blood for one particular moment in time, a measurement that is known to have wide day-to-day variability. The omega-3 index, which measures both EPA and DHA within red blood cells, is a much more accurate indicator of long-term omega-3 intake and tissue status than is the plasma omega-3 level, which is subject to significant day-to-day variability. They also failed to account for body weight, a factor highly associated with prostate cancer (and more of the prostate cancer group was overweight). It is suggested that fat cells release inflammatory cytokines, and increased inflammation is a suspected cause of prostate cancer. Many factors contribute to omega 3 blood levels, including other dietary factors, metabolism, genetics etc., and some of the things not taken into consideration included that more than 50% of the prostate cancer group were smokers, consumed alcohol, and were overweight.
Anthony Victor D'Amico, MD, PhD, who specializes in prostate cancer research, notes that while the study adjusted for diabetes and family history, they left out huge factors associated with prostate cancer, such as race, age, PSA level, rectal exam, body mass index, and whether or not they were overweight (already mentioned to be highly correlated). According to Dr. D'Amico, unless you take these things into consideration, "You could associate almost anything with prostate cancer; something like "driving a Cadillac" could be associated with prostate cancer if you don't account for the major factors that cause prostate cancer." Dr. D'Amico also finds it interesting that Table one in the study lists the PSA level and race but those factors were not adjusted for in the model, "maybe because the association was lost once they did."
Even if the blood measurement of fatty acids was a gold standard, which it is not, the clinical relevance of such small differences (.04% EPA and 0.1% DHA) in each of the groups remains unknown. Dr. Don Bellgrau, an NIH grant reviewer, emphasizes that the assay is quite cumbersome and prone to error, for which they provide no data regarding validation. It involves extracting total lipids from plasma followed by separation of other lipids by chromatography. Most biomarker people would say the more you do to the sample prior to analysis the more likely you are to add error to the process. They also use pooled serum from "healthy volunteers as an internal control for each assay but do not show any data regarding day to day variability when assaying the same samples. They also express fatty acids as a weight percentage of total phospholipid fatty acids, rather than an absolute value, and using percentages is likely to be misleading."
Dr. Bellgrau further explains how the authors of the article even stated within the article that analyzing in this manner could lead to spurious (false) conclusions. He points out that the authors admit that "because some fatty acids represent greater proportions of the total weight than others"(page 4), they did some statistical gymnastics to make the claim that this was a valid approach even though they state later that "spurious associations arise because of measurement of fatty acids as a proportion of total weight rather than absolute concentration" (page 6). This approach is likely what gave them their conclusion (potentially spuriously) because as they state on page 8 'expressing fatty acids as weight proportions could create spurious associations because an increase in the percentage of one type of fatty acid requires a decrease in others". Dr. Bellgrau emphasized that they should have compared by absolute weight, not by percentage.
Another expert who questions the validity of inferring causality from observations that don't take confounding factors into consideration is Michael Savage, PhD. Dr. Savage's PhD is in epidemiology from U of C Berkeley, and he interviews Anthony Victor
D'Amico MD, PhD (discussed above) about this "bogus study" reporting "junk science" in the following video:
http://www.michaelsavaqe.wndcom/wp-incjudes/ms-thes.ijhp?fiIe=201 3/07/071113-FISH-OILINTERVIEW.mD3
Dr. Savage notes that in addition to not measuring fish intake or supplement intake, there was no consideration for what quality of fish (fresh water fish?) or supplements (molecularly distilled and purified, free of toxins?), the duration of exposure to omega 3's, and whether or not subjects started taking fish oil before or after they were diagnosed with prostate cancer. Given that many people who have heard about the benefits of fish oil would want to supplement with it after a diagnosis, the study does not consider that the prostate cancer group may have intentionally increased their consumption of omega 3's.
A 2010 study led by the same researcher reported that the use of fish oil supplements was NOT associated with any risk for prostate cancer...
"Although there is evidence from studies of prostate cancer cell lines and rodent models that several supplements may have antiinflanimatory, antioxidant, or other anticancer properties, few epidemiologic studies have examined the association between nonvitamin, nonmineral, "specialty" supplement use and prostate cancer risk." They then reported on participants, 50-76 yr, who were 35,239 male members of the VITamins and Lifestyle (VITAL) cohort who were residents of western Washington state, and who completed an extensive baseline questionnaire in 2000-2002. Participants responded about their frequency (days/wk) and duration (yr) of specialty supplement uses. 1,602 incident invasive prostate cancers were obtained from the Surveillance, Epidemiology, and End Results registry. No correlation with fish oil and prostate cancer was observed".
In fact, a 2010 meta-analysis (analysis of many clinical trials and much much stronger than any "observational" study), "showed a significant 63% reduction in prostate cancer-specific mortality"." Additionally, over 45,000 men were studied by Augustssonm K et al., and they found that: "Each additional daily intake of 0.5 g of marine fatty acid from food was associated with a 24% decreased risk of metastatic cancer. We found that men with high consumption of fish had a lower risk of prostate cancer, especially for metastatic cancer. Marine fatty acids may account for part of the effect, but other factors in fish may also play a role."
Also, it is not a trivial fact that high omega-3 levels are associated with lower rates of death from any cause". Clearly, the benefit of fish oils in the literature remains favorable, and will survive a weak attempt in the mass media to sensationalize a poorly deduced conclusion.
References:
J Natl Cancer Inst. 2013 Jul 10. Plasma Phospholipid Fatty Acids and Prostate
Cancer Risk in the SELECT Trial. Brasky TM, Darke AK, Song X, Tangen
CM, Goodman PJ, Thompson IM, Meyskens FL Jr. Goodman GE, Minasian LM, Parnes HL, Klein EA, Kristal AR.
ii Nutr Cancer. 2011;63(4):573-82. Specialty supplements and prostate cancer risk in the VITamins and Lifestyle (VITAL) cohort. Brasky TM, Kristal AR, Navarro SL, Lampe JW, Peters U, Patterson RE, White E.
iii Am J Clin Nutr. 2010 Nov;92(5):1223-33. Fish consumption and prostate cancer risk: a review and meta-analysis. Szymanski KM, Wheeler DC, Mucci LA.
iv Cancer Epidemiol Biomarkers Prev. 2003 Jan; 12(l):64-7. A prospective study of intake of fish and marine fatty acids and prostate cancer. Augustsson
K, Michaud DS, Rimm EB, Leitzmann MF, Stampfer MJ, Willett WC, Giovannucci E.
Mozaffarian D, Lemaitre RN, King IB, Song X, Huang H, Sacks FM, Rimm EB, Wang M, Siscovick DS. Plasma Phospholipid Long-Chain omega-3 Fatty Acids and Total and Cause-Specific Mortality in Older Adults: A Cohort Study. Annals of internal medicine 2013;158:515-25; Pottala jV, Garg S, Cohen BE, Whooley MA, Harris WS. Blood Eicosapentaenoic and Docosahexaenoic Acids Predict All-Cause Mortality in Patients With Stable Coronary Heart Disease: The Heart and Soul Study. Circulation Cardiovascular quality and outcomes 2010;3:406-12.
Nutri-West is a well-respected company that offers high quality fish oil, pharmaceutical grade, molecularly distilled (to remove toxins), that is technically formulated to the best EPA/DHA ratios according to the scientific literature. It is called the Complete line of omega 3's: Complete Omega 3 Essentials 2:1 capsules, Complete Hi-Potency Omega 3 Liquid, and Complete Children's DHA/EPA Chewables. Al! fish oil is recommended with co-factors to increase absorption/utilization, and to protect against oxidation.
Courtesy of:
John H. Keefe III, D.C.
(918) 663-1111
WELLNESS: THE MANY HEALTH BENEFITS OF AVOCADOS Avocados have a long list of potential health benefits. For example, besides its anti-inflammatory properties, previous research from Japan suggests this powerful fruit may also help protect against liver damage. Due to its beneficial raw fat content, avocado enables your body to more efficiently absorb fat-soluble nutrients (such as alpha- and beta-carotene and lutein) in other foods eaten in conjunction. Contain compounds that appear to inhibit and destroy oral cancer cells Can help improve lipid profiles in both healthy individuals and those with non optimized HDL/ total cholesterol levels). In one study,8 healthy individuals saw a 16 percent decrease of serum total cholesterol level following a one-week long diet high in monounsaturated fat from avocados. In those with elevated cholesterol levels, the avocado diet resulted in a 17 percent decrease of serum total cholesterol, and a 22 percent decrease of both LDL-cholesterol and triglycerides, along with an 11 percent increase of the so-called “good” HDL cholesterol.