



Antidepressant use has become increasingly common, often extending for many years or even decades. Many patients are told these medications are safe, effective, and essential for long-term mental health. However, emerging research suggests that long-term antidepressant use may carry under-recognized cardiovascular risks, including an increased risk of sudden cardiac death.
Sudden cardiac death is a rapid and often fatal collapse caused by a sudden loss of effective heart rhythm. It typically occurs within minutes and frequently without warning. In younger adults, it is most often linked to electrical rhythm disturbances or cardiomyopathy; in older adults, it is commonly associated with coronary artery disease. Regardless of age, the outcome is usually the same.
Recent population-level data suggest that antidepressant exposure may be contributing to a shift in this risk profile.
Research presented at the 2025 European Heart Rhythm Association annual meeting examined antidepressant exposure and sudden cardiac death using national registry data from Denmark.¹ The study reviewed all deaths among adults aged 18 to 90 living in Denmark in 2010.
Out of 45,701 total deaths, 6,002 were classified as sudden cardiac deaths. Researchers then analyzed antidepressant prescription history over the prior 12 years.
Participants were considered exposed if they had filled at least two antidepressant prescriptions within a single year. Exposure was categorized as:
Compared with individuals who had never used antidepressants:
Importantly, the risk increased progressively with duration of use, suggesting a time-dependent relationship rather than a transient effect.
The association was not limited to older adults.
For adults aged 18–29 and 80+, the increase was not statistically significant, possibly due to smaller sample sizes.
Across age groups, longer exposure consistently correlated with higher risk, indicating a dose-response relationship over time.
According to study authors, several biological and behavioral factors may contribute:
These mechanisms are not mutually exclusive and may compound over time.
Antidepressants remain widely prescribed despite ongoing debate about their effectiveness for most patients.
For many individuals, symptoms such as sadness, anxiety, or burnout may reflect nutritional deficiencies, circadian disruption, inflammation, or psychosocial stress, rather than a primary chemical imbalance.
Antidepressants should never be stopped abruptly. Anyone considering discontinuation should work with a qualified healthcare provider experienced in tapering protocols.
Resources that may be helpful include:
Gradual tapering supports nervous system stability and reduces withdrawal risks.
In cases of suicidal ideation or crisis, immediate medical help is essential. In the U.S., call 988 or go to the nearest emergency room.
Research supports multiple non-pharmacologic strategies that address mood at the biological level:
Antidepressants may help a small subset of patients, but long-term use is not without risk, particularly for cardiovascular health. The emerging association with sudden cardiac death underscores the importance of periodic reassessment, informed consent, and exploration of root-cause approaches.
Mental health care should aim to restore biological balance—not simply suppress symptoms—while minimizing long-term harm.
to order:
https://us.fullscript.com/welcome/jkeefe-dc
Many people seeking better metabolic health are interested in natural strategies that help manage blood sugar levels and support a healthy weight. Reducore™ is designed as a multifaceted nutritional blend that targets several physiological processes linked to glucose regulation, satiety, and metabolic resilience.
In this article, we explain how Reducore™ works based on its ingredients, what the research says, and how it may complement lifestyle approaches for metabolic support.
What Is Reducore™?
Reducore™ is a metabolic health supplement formulated to support:
It combines resistant fibers, functional carbohydrates, targeted plant extracts, amino acids, and magnesium. These ingredients act through distinct metabolic pathways that influence digestion, glucose uptake, and energy utilization.
Key Ingredient Groups and How They Work
1. BiomeFuel Blend – Supporting the Gut–Metabolism Axis
The BiomeFuel Blend includes resistant fibers and functional carbohydrates that act as prebiotics, nourishing beneficial gut microbes.
2. Muscle Support Blend – Promoting Lean Body Composition
Maintaining lean muscle is important because muscle tissue is a major site of glucose utilization.
3. Glycemic Control Blend – Supporting Balanced Carbohydrate Processing
This blend contains plant extracts traditionally studied for their effects on glucose metabolism:
How Reducore™ May Support Blood Sugar and Weight Goals
Reducore™ targets multiple, interrelated pathways important for metabolic health:
Because it addresses several mechanisms, Reducore™ may be more effective than single-ingredient products at supporting metabolic resilience.
Practical Use Considerations
To order click link
https://us.fullscript.com/welcome/jkeefe-dc
Conclusion
Reducore™ is a thoughtfully formulated supplement that combines clinically studied fibers, plant extracts, amino acids, and magnesium to support balanced metabolic function. Its multi-ingredient approach aligns with current understanding of glucose metabolism, gut health, and lean body composition. When paired with a healthful lifestyle, it may help individuals seeking to support blood sugar control and weight management.
References (for publication)
Managing type 2 diabetes is often framed around diet, exercise, and medication. Emerging research suggests that another, often overlooked factor may play a meaningful supporting role: daily exposure to natural daylight.
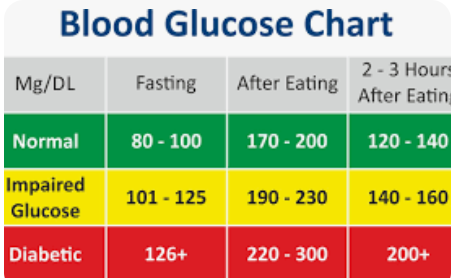
A recent study published in Cell Metabolism found that people with type 2 diabetes who were exposed to natural daylight—even while indoors near a window—showed more stable blood sugar patterns and improved metabolic signaling compared to those exposed only to typical artificial lighting.
Modern lifestyles keep most people indoors under artificial light for 80–90% of the day. These lights are far dimmer and biologically flatter than sunlight and provide weak signals to the body’s internal clock, known as the circadian rhythm.
Circadian rhythms regulate:
When this internal clock becomes misaligned—common in shift work, late nights, and indoor lifestyles—insulin resistance and blood sugar instability tend to worsen, two hallmark issues in type 2 diabetes.
Researchers studied 13 adults with type 2 diabetes in a controlled office environment over two separate 4.5-day periods.
This metabolic pattern is associated with better insulin sensitivity and glucose control.
Daily daylight exposure acts as a master reset for the body’s metabolic timing.
Helpful strategies include:
These habits help align insulin release and glucose uptake with the body’s natural rhythms.
Circadian alignment works best when paired with proper meal timing:
This complements daylight exposure by reinforcing the same metabolic signals.
The study found that daylight exposure shifted metabolism toward fat utilization rather than carbohydrate overuse—a favorable pattern in type 2 diabetes.
Nutritional strategies that support this include:
These approaches help smooth blood sugar curves rather than forcing sharp insulin responses.
Better synchronization of cellular clock genes improves how cells respond to insulin.
Supporting factors include:
Daylight exposure is not a replacement for diabetes medication, diet, or exercise. The researchers emphasize that it should be viewed as a supportive lifestyle factor, not a standalone treatment.
However, the findings highlight an important point: blood sugar control is not governed by food alone. Light exposure, timing, sleep, and daily rhythm all influence how the body processes glucose.
Something as simple as sitting near a window or spending more time outdoors during the day may help people with type 2 diabetes:
When combined with nutritional strategies, proper meal timing, and consistent daily routines, supporting the body’s natural circadian rhythm can become a valuable part of a comprehensive, natural approach to blood sugar management.
Sometimes, better metabolic health begins not with another intervention—but with restoring the signals the body was designed to follow.

For many people, heartburn is dismissed as a minor inconvenience. But when acid reflux becomes frequent or chronic, it can set off a chain of events that may lead to esophageal inflammation, Barrett’s esophagus, and increased cancer risk.
The encouraging news is that addressing reflux early—at the functional and nutritional level—can interrupt this progression before structural damage occurs.
Acid reflux occurs when the lower esophageal sphincter (LES)—the “acid gate” between the stomach and esophagus—fails to stay closed. This allows stomach contents to travel upward into tissue that was never designed to tolerate acid.
At this stage, reflux is often functional and reversible.
Key strategies include:
Adequate minerals, proper digestion, and nervous-system regulation often restore normal acid direction without suppressing stomach acid.
Repeated acid exposure causes ongoing irritation, inflammation, and erosion of the esophageal lining—essentially a slow chemical injury.
The focus here shifts to soothing tissue, reducing inflammation, and improving mucosal defense, including:
By reducing repeated injury, the body is given the opportunity to heal rather than adapt pathologically.
When acid exposure continues, the esophagus may adapt by replacing normal esophageal cells with stomach-like cells—a process called metaplasia, known clinically as Barrett’s esophagus.
This is not cancer, but it is a precancerous condition that increases long-term risk.
At this stage, the goal is to stop progression, not ignore the condition.
Supportive strategies may include:
While cellular changes require medical oversight, functional care aims to remove the ongoing insult that drives further mutation.
If cellular changes continue unchecked, dysplasia may develop, representing a higher-risk state prior to cancer.
At this stage, medical management is essential, but nutritional and lifestyle strategies still play a supportive role by:
Natural approaches do not replace medical care here—but they can complement it by addressing systemic contributors.
Persistent reflux should never be ignored, especially when accompanied by:
Nighttime reflux is particularly concerning due to prolonged acid exposure during sleep.
Heartburn is not the problem—directional acid flow is.
When addressed early, nutritional therapy, mineral support, meal timing, and natural digestive regulation can often correct reflux before permanent tissue changes occur. Once changes progress, early intervention still matters, as stopping ongoing injury reduces future risk.
Digestive health is not just about suppressing symptoms—it’s about restoring proper function before adaptation turns into disease.

For decades, dietary advice around brain health has leaned heavily toward low-fat recommendations. A new long-term Swedish study, however, adds nuance to that narrative—suggesting that certain fermented, higher-fat dairy products, particularly cheese and cream, may be associated with a lower risk of dementia, while others show no benefit or even potential risk.
Researchers analyzed data from the Malmö Diet and Cancer cohort, following 27,670 adults aged 45–73 for an average of 25 years. Detailed dietary assessments were conducted at baseline, including food diaries, interviews, and questionnaires. Dairy intake was categorized by type and fat content.
During follow-up, 3,208 participants developed dementia, including Alzheimer’s disease (AD) and vascular dementia (VaD).
The study adjusted for numerous confounders, including age, sex, education, smoking, physical activity, alcohol use, BMI, hypertension, overall diet quality, and other dairy intake.
It is important to be clear: this was an observational study. It cannot prove cause and effect. Diet was measured only once, cognitive status at baseline was not assessed, and dementia diagnoses after 2014 were not fully validated.
In other words, this study does not demonstrate that eating cheese or cream prevents dementia.
What it does show is a consistent association that challenges the idea that higher-fat dairy is automatically harmful—and that not all dairy products behave the same metabolically or neurologically.
A critical pattern emerges when the results are viewed carefully:
The potentially protective associations are specific to fermented dairy, not dairy fat in general.
Butter—despite being high in fat—showed an opposite association. Milk and low-fat dairy were largely neutral.
This points to the food matrix, not just fat content, as the relevant variable.
Fermented dairy products contain compounds that non-fermented products lack, including:
These factors are increasingly studied for their roles in vascular health, inflammation, and gut–brain interactions—all relevant to dementia risk, especially vascular dementia.
While this Swedish cohort focused largely on hard, fermented cheeses typical of Scandinavian diets, similar mechanisms may plausibly apply to other fermented dairy products, including:
That said, not all fermented dairy is equivalent. Sugar content, processing, bacterial strains, and fermentation duration matter—and results from one population cannot automatically be generalized to others.
One of the most important findings is that the reduced Alzheimer’s risk associated with high-fat cheese was seen only in people without the APOE ε4 allele, a known genetic risk factor for Alzheimer’s disease.
This strongly argues against one-size-fits-all dietary advice and supports a personalized nutrition approach, particularly for brain health.
This study does not overturn existing dietary guidance, nor does it justify recommending high-fat dairy as a preventive treatment for dementia.
What it does do is:
As the authors themselves note, cheese and cream are likely markers of a broader dietary and lifestyle pattern, rather than magic bullets.
In nutrition—as in neuroscience—context matters.
Week of: Monday July 28, 2025
Courtesy of:
John H. Keefe III, D.C.
(918) 663-1111
IN THE NEWS: Abdominal Fat Increases Psoriasis Risk in Women Psoriasis affects over 7.5 million adults in the U.S. and is now recognized as a full-body inflammatory disease, not just a skin disorder. New research shows that abdominal fat is a stronger predictor of psoriasis risk than overall body fat, especially in women. Even without genetic risk factors, women with high waist-to-hip ratios had increased psoriasis risk, proving lifestyle plays a major role in disease development. A separate 14-year study found that women who gained more weight over time — particularly around the abdomen — had a significantly greater chance of developing psoriatic arthritis. These findings confirm that reducing central obesity is a powerful, proactive step to reduce inflammation and lower your risk of both psoriasis and joint damage. Abdominal fat is more than a cosmetic concern — it’s a metabolic and immune disruptor. In conditions like psoriasis, targeting abdominal fat loss through diet, exercise, and metabolic support may be more important as any topical or pharmaceutical treatment. JAMA Dermatol. 2021;157(8):940-946--Journal of Investigative Dermatology, May 27, 2025--Science Daily, May 27, 2025--News-Medical.net, May 27, 2025
WELLNESS: "Ultraviolet (UV) light has well-documented antimicrobial properties and is widely used in sterilization and disinfection of surfaces, air, and water. UVB light also plays a crucial role in human health by stimulating the production of vitamin D in the skin, which is essential for bone health, immune function, and overall well-being. The Sunshine Spectrum: Using Ultraviolet Light Wisely--Ultraviolet (UV) light often gets a bad reputation—and for good reason when it’s overused. But like many natural tools, UV light can be a powerful force for good when used correctly. The Bright Side of UV Light, Vitamin D Boost – Just 5–15 minutes of sunshine on the arms and legs, a few times a week, can help your body produce this critical vitamin that supports bones, immunity, and mood. Mood and Sleep Support – UV exposure helps regulate your body’s natural sleep-wake cycle and may reduce symptoms of seasonal depression. Purification Uses – In safe, controlled settings, UV light is used to sterilize air, water, and surfaces—destroying harmful viruses and bacteria. The Risks of Overexposure, Skin Damage & Cancer Risk – Unprotected, prolonged sun exposure can lead to sunburn, premature aging, and increased risk of skin cancer. Eye Damage – UV light can harm the eyes over time, contributing to cataracts and other conditions. Safe & Smart UV Use, Enjoy sun responsibly—short, direct exposures during early morning or late afternoon hours are best. Antioxidant-rich foods (e.g., berries, tomatoes, leafy greens, green tea, and omega-3s) improve the skin’s ability to handle UV stress. Supplements like astaxanthin, vitamin C, and vitamin E have shown potential in supporting skin protection from within. Avoid tanning beds—they deliver high doses of UV radiation with serious health risks and little real benefit. Limit direct sun exposure during peak UV hours (typically 10 AM to 3 PM). Opt for early morning or late afternoon sun to gain benefits like vitamin D with less risk.
CHIROPRACTIC: Why Parents Are Turning to Chiropractic for Their Children When 4-year-old Mason kept getting ear infections, his mom Sarah grew tired of endless antibiotics. A neighbor suggested chiropractic care. Skeptical but desperate, she took him in—and within a few gentle treatments, the infections stopped. “I realized chiropractic wasn’t just about pain relief—it was about helping the body function better,” Sarah says. She’s not alone. More parents are choosing chiropractic care to help with common childhood conditions like: Ear infections--Colic and reflux—Constipation--Allergies and asthma--Postural issues and scoliosis. How It Works Chiropractic focuses on the nervous system. When spinal misalignments—called subluxations—interfere with nerve signals, they can contribute to many childhood health challenges. Gentle adjustments restore balance and allow the body to heal naturally. A study in the Journal of Manipulative and Physiological Therapeutics confirmed pediatric chiropractic care is both safe and effective, especially when performed by trained practitioners (Alcantara et al., 2009). Dr. Jeanne Ohm of the ICPA wrote: “Correcting nervous system interference helps the body function at its best. That’s what chiropractic offers children.” If your child struggles with recurring health issues—or you simply want to support their healthy development—chiropractic may be the natural, drug-free answer you’ve been looking for. https://icpa4kids.org/-- https://pubmed.ncbi.nlm.nih.gov/19480843/-- https://icpa4kids.org/Chiropractic-Research/ear-infections.html-- https://www.nccih.nih.gov/health/spinal-manipulation-what-you-need-to-know
FUNNY BONE: Unintentionally Funny Doctor Notes--"Patient has left white blood cells at another hospital."--"On the second day, the knee was better, and on the third day it disappeared."--"Patient was alert and unresponsive." (A Schrödinger’s diagnosis?)--"Skin: somewhat pale but present."--"The patient refused autopsy." (Good call, considering.)--"The patient has no previous history of suicide."--"She is numb from her toes down."--"Occasional, constant infrequent headaches."--"The patient lives at home with his mother, father, and pet turtle, who is presently enrolled in daycare three times a week."--"Discharge status: alive but without my permission." “Out of the Mouths of Babes…” 1. Q: What ended in 1896? A: 1895.--2. Q: Explain why the diagram below is a bar graph. A: Because it has bars.--3. Q: Name six animals that live specifically in the Arctic. A: Two polar bears and four seals.--4. Q: What is the highest frequency noise a human can register? A: Mariah Carey.
| Visit Visit our web sites: keefeclinic.com & keefeclinic.quora.com |

New Study Highlights Risk-Based Screening — and the Role of Nutrition in Breast Health
A large new clinical trial published in the Journal of the American Medical Association (JAMA) is raising an important question: Do all women need annual mammograms, or should screening be tailored to individual risk?
The study does not suggest abandoning mammograms. Instead, it points toward a more personalized approach — while also reminding us that screening is only one part of breast-cancer prevention. Nutrition, inflammation control, metabolic health, and hormone balance play critical roles as well.
Overview of the Study: The WISDOM Trial
The WISDOM (Women Informed to Screen Depending on Measures of Risk) trial followed over 28,000 women aged 40–74 across the U.S.
Participants were divided into two groups:
Standard Screening Group
Risk-Based Screening Group
Screening recommendations were based on:
Based on risk:
Key Findings
Researchers concluded that risk-based screening was as safe as annual screening when measuring late-stage cancer outcomes.
Why Some Experts Urge Caution
Radiologists point out an important limitation:
The study did not fully assess whether early-stage cancers (stage 0–2A) were detected as effectively.
Over 60% of breast cancers are diagnosed at early stages, where cure rates exceed 90%. Detecting cancer earlier, not merely avoiding late-stage disease, is the primary value of screening.
Additionally, labeling women under 50 as “low risk” may be problematic, as breast cancer rates are rising in younger women.
Breast Health Is More Than Imaging
Regardless of screening frequency, breast-cancer risk is strongly influenced by metabolic, inflammatory, and hormonal factors — many of which are modifiable.
Nutritional Therapy for Breast Health
A breast-protective nutritional strategy focuses on reducing inflammation, improving estrogen metabolism, and supporting immune surveillance.
Key Dietary Principles
Nutrients That Support Breast Tissue and Cellular Health
All supplementation should be individualized, especially for women with prior breast findings.
Lifestyle Factors That Matter as Much as Screening
Bottom Line
Risk-based mammography may be a safe alternative to annual screening for some women — but it does not replace the importance of early detection.
More importantly, screening alone does not prevent cancer. A comprehensive approach that includes nutrition, lifestyle, metabolic health, and individualized screening decisions offers the greatest long-term protection.
Women should make screening decisions in partnership with their healthcare provider, considering both imaging and modifiable risk factors.
Keefe Clinic
5016 S. 79th E. Avenue
Phone: 918-663-1111
Fax: 918-663-2129
Email: docjohn@keefeclinic.com

What They Are — Why They Form — How to Treat Them Safely
What Is a Corn?
A corn is an area of thickened, hardened skin that develops in response to repeated pressure or friction. Corns are the body’s way of protecting itself — but they can become painful and limit walking if left untreated.
Corns most commonly appear:
Why Corns Form (Root Cause)
Corns do not form randomly. They are caused by ongoing mechanical stress such as:
Important:
If the pressure is not corrected, the corn will return — even if it is removed.
The 5 Key Elements of Treating Corns
1. Remove or Reduce Pressure (MOST IMPORTANT)
This is the foundation of treatment.
Helpful steps:
Without pressure relief, treatment will fail.
2. Soften the Hardened Skin
Daily foot care helps reduce thickness safely.
This makes the corn easier to manage and less painful.
3. Gently Reduce Thickness (DO NOT CUT)
After soaking:
⚠️ Do not cut, shave, or dig into a corn. This can cause infection.
4. Keep the Skin Soft and Healthy
Apply a moisturizing agent daily:
This prevents cracking and reduces irritation.
5. Monitor for Warning Signs
Seek professional care if you notice:
What NOT to Do
⚠️ Do NOT self-treat corns if you have:
These patients should always be evaluated professionally.
Corns vs. Calluses (Quick Difference)
Long-Term Prevention
Corns are often a mechanical problem, not just a skin problem.
Summary
Corns can usually be managed safely by reducing pressure, softening the skin, and gently maintaining the area. Long-term relief depends on correcting the cause — not just treating the surface.
Keefe Clinic
5016 S. 79th E. Avenue
Phone: 918-663-1111
Fax: 918-663-2129
Email: docjohn@keefeclinic.com

How everyday food choices shape long-term health
One of the most powerful tools for protecting long-term health does not come from a prescription pad or a medical procedure. It comes from the food choices made every day.
Large population studies consistently show that diet plays a major role in cancer risk, particularly cancers of the digestive tract, breast, uterus, kidney, and liver. In the United States alone, researchers estimate that tens of thousands of cancer cases each year are associated with poor dietary patterns — not genetics, not random chance, but long-term nutritional stress on the body.
Modern diets are increasingly dominated by:
These foods tend to promote:
Each of these factors has independently been linked to increased cancer risk.
Excess body fat is not inert. Fat tissue acts like an endocrine organ, influencing hormones, inflammatory signaling, and immune function. Obesity has been associated with increased risk for at least 13 different types of cancer, including colorectal, postmenopausal breast, uterine, kidney, liver, and pancreatic cancers.
Sugar-sweetened beverages are one of the fastest ways to drive weight gain and metabolic dysfunction, while providing little to no nutritional benefit.
Whole, natural foods help support the body’s built-in defense and repair systems. Diets rich in:
provide:
Fiber plays a particularly important role by feeding beneficial gut bacteria, reducing inflammatory byproducts, and helping the body eliminate excess hormones and metabolic waste.
Rather than focusing on restriction, a better approach is replacement.
Eat more of:
Eat less of:
This type of diet supports:
Cancer does not develop overnight. It reflects years of biological stress, inflammation, and imbalance. The encouraging reality is that consistent, modest dietary changes can significantly influence long-term risk.
Food does not guarantee perfect health, but it strongly shapes the internal environment in which health or disease develops.
You do not need extreme diets or fear-based nutrition rules. You need:
Eating well is not about perfection. It is about giving your body the raw materials it needs to repair, defend, and regulate itself naturally.
Dr. John H. Keefe III, DC
Keefe Clinic
5016 S. 79th E. Avenue
Tulsa, OK 74145
Phone: 918-663-1111
Fax: 918-663-2129
Email: docjohn@keefeclinic.com

A stroke is a true medical emergency. Brain tissue depends on a constant supply of oxygenated blood, and when that supply is interrupted—even briefly—permanent damage can occur. Rapid recognition and immediate emergency care can be the difference between recovery and lifelong disability.
Legitimate Stroke Warning Signs
The following symptoms are well-established in neurology and emergency medicine and should prompt an immediate call to 911:
These are not subtle symptoms and should never be ignored.
Simple At-Home Stroke Screening Tests (FAST and Beyond)
You are already using several clinically valid screening maneuvers. Here is the complete, evidence-based set, including the ones you mentioned:
1. Arm Drift Test
Ask the person to raise both arms straight out and hold them up.
2. Facial Smile Test
Ask the person to smile.
3. Speech Test
Ask the person to repeat a simple sentence.
4. Cheek Puff / Air-Hold Test (what you already do)
Ask them to puff out their cheeks or hold air in their mouth.
5. Tongue Deviation Test
Ask them to stick out their tongue.
6. Hand Grip Strength Test
Ask them to squeeze both of your hands.
7. Eye Gaze Test
Ask them to follow your finger with their eyes.
The FAST Rule (Public Health Standard)
Most emergency medicine uses the FAST acronym:
Time matters. Do not drive yourself or wait to see if symptoms pass.

Every year around Christmas and New Year’s, hospitals see a predictable spike in heart attacks and heart rhythm disturbances. In fact, cardiologists report that Christmas Eve is the single highest-risk day of the year for cardiac events.
This seasonal pattern is so consistent it has a name: Holiday Heart Syndrome.
Holiday heart syndrome is driven less by cold weather alone and more by temporary but intense lifestyle changes, including:
These factors increase inflammation, thicken the blood, disrupt electrolytes, raise blood pressure, and stress the nervous system — all of which can trigger atrial fibrillation, plaque rupture, or even heart attack.
Cold weather adds another layer by causing vasoconstriction (narrowing of blood vessels), which raises cardiac workload and increases risk when inflammation is already high.
While cholesterol has long been blamed for heart disease, modern research increasingly shows that chronic inflammation is the true driver. Cholesterol often appears at sites of arterial injury as part of the body’s repair response.
During the holidays, inflammatory load rises rapidly due to:
This inflammatory surge destabilizes plaques and disrupts heart rhythm — explaining why cardiac events cluster around holidays.
The good news: holiday heart syndrome is largely preventable. Small, consistent actions can dramatically lower risk.
Dehydration thickens the blood and worsens arrhythmia risk. Aim for steady water intake throughout the day, especially if consuming alcohol or salty foods.
Magnesium and potassium are critical for normal heart rhythm. Deficiency increases the risk of atrial fibrillation and palpitations.
Natural sources include:
Omega-3s reduce inflammation, stabilize heart rhythms, and improve blood vessel function.
Sources include:
Low omega-3 levels are associated with arrhythmias, heart attacks, and sudden cardiac death.
You don’t need a full workout routine. 5,000–10,000 steps per day, light resistance exercises, or short walks after meals help regulate blood sugar, blood pressure, and inflammation.
Movement also lowers stress hormones.
Binge drinking is one of the strongest triggers for holiday atrial fibrillation. Alcohol directly irritates heart tissue and depletes magnesium.
If drinking, keep intake modest and alternate with water.
Stress is not just emotional — it is neurological. Techniques that calm the autonomic nervous system reduce heart strain:
Chronic sympathetic (“fight or flight”) dominance is strongly linked to heart disease and rhythm disorders.
Holiday heart events are not random. They are the predictable result of temporary inflammation overload combined with stress, dehydration, and rhythm disruption.
Protecting your heart during the holidays doesn’t require perfection — just awareness and balance. Small steps taken consistently can dramatically reduce risk and help you enjoy the season with peace of mind.
If you have a history of palpitations, arrhythmia, high blood pressure, or heart disease — or if you want a more personalized, natural approach to cardiovascular health — speak directly with Doctor Keefe.
Keefe Clinic
5016 S. 79th E. Avenue
Phone: 918-663-1111
Fax: 918-663-2129
Email: docjohn@keefeclinic.com
A recent global analysis published in Nutrition Research Reviews found that approximately 76% of people worldwide are deficient in omega-3 fatty acids, particularly EPA and DHA—two fats essential for cardiovascular health. This widespread deficiency may help explain why heart disease remains the leading cause of death, despite decades of focus on cholesterol levels alone.
Omega-3 fatty acids play a critical role in regulating inflammation, stabilizing heart rhythms, lowering triglycerides, supporting blood vessel health, and protecting brain and eye function. When omega-3 intake is low, inflammation tends to rise—setting the stage for arterial damage, plaque instability, and increased cardiovascular risk.
Inflammation: the real driver of heart disease
For many years, cholesterol was framed as the primary cause of heart disease. We now know the picture is more complex. Cholesterol itself is not inherently harmful—it is a repair molecule the body uses to patch damaged blood vessels. The real problem is why those vessels are damaged in the first place.
That culprit is chronic inflammation.
Inflammation injures the arterial lining, making it vulnerable to plaque formation. Cholesterol then accumulates at those injury sites, not as the cause, but as part of the body’s attempted repair process. Without addressing inflammation, simply lowering cholesterol does not resolve the underlying problem.
Omega-3 fatty acids are among the most powerful dietary anti-inflammatory agents known. Adequate levels help calm inflammatory signaling, improve endothelial function, and reduce the risk of clot formation and arrhythmias.
Food sources and supplementation
The richest natural sources of EPA and DHA are oily fish, including salmon, sardines, mackerel, herring, anchovies, and trout. Many people benefit from eating these fish several times per week. For those who do not consume fish regularly, high-quality omega-3 supplements can be helpful, ideally guided by lab testing such as the omega-3 index.
An omega-3 index around 8% is associated with lower cardiovascular risk, while levels below 4% are considered low.
Other anti-inflammatory foods that support heart health
Omega-3s work best as part of a broader anti-inflammatory diet. Helpful foods include:
The takeaway
Heart disease is not simply a cholesterol problem—it is primarily an inflammatory problem. Omega-3 deficiency is widespread and directly contributes to that inflammatory burden. Correcting it, alongside an anti-inflammatory diet and lifestyle, addresses the root cause rather than chasing numbers on a lab report.
Reducing inflammation restores balance. And balance is where true heart health begins.

As a new, more aggressive flu strain circulates this winter, many people are asking an important question: Is relying on the flu shot alone enough? Increasingly, both doctors and independent researchers are saying the answer is no — especially when vaccine effectiveness is inconsistent and immune systems are already under strain.
What Doctors Say About This Year’s Flu
Medical experts agree that this flu season is shaping up to be difficult. The dominant strain, Influenza A (H3N2, subclade K), has been associated with more severe symptoms and faster spread. Public health officials continue to recommend vaccination, noting that it may reduce hospitalization and severity for some individuals.
However, even physicians acknowledge a key limitation: this year’s vaccine is not a strong match for the dominant strain, which may reduce its overall effectiveness.
“The vaccine is important, but because it’s not perfectly aligned with this variant, that may be contributing to the severity of cases we’re seeing.”
— Dr. Neil Maniar, Northeastern University, Public Health
Independent Research Raises Important Questions
Independent reviews of flu vaccine performance over many years show that consistent, high-level protection has been elusive.
A widely cited BMJ review concluded:
“Evidence for consistent high-level protection is elusive.”
— BMJ, 2012;345:e7856
The same analysis found that while the flu vaccine may offer modest protection in young, healthy adults, evidence of strong protection in older adults — who account for the majority of flu-related deaths — is limited.
A Cochrane Database systematic review also found that vaccinating healthcare workers did not significantly reduce laboratory-confirmed influenza in elderly nursing-home residents, calling into question claims that widespread vaccination alone reliably protects vulnerable populations.
(Cochrane Database of Systematic Reviews, 2010; CD005187)
These findings do not mean the flu shot has no value — but they do suggest that vaccination alone is not sufficient, especially in years of strain mismatch.
Why Immune Resilience Matters More Than Ever
Instead of viewing immunity as something delivered by a single intervention, many clinicians are emphasizing direct immune system support — strengthening the body’s ability to respond effectively to infection.
This approach does not replace medical care, but complements it, particularly during high-stress, low-sleep winter months.
Natural Healthcare Strategies That Support Immune Function
1. Prioritize Sleep (Non-Negotiable)
Sleep is one of the strongest predictors of immune response. Studies show that people who sleep less than six hours per night are significantly more likely to get sick after viral exposure.
2. Support Nutrition — Especially Protein and Micronutrients
Immune cells are protein-dependent and micronutrient-dependent.
Key nutrients include:
Whole foods — eggs, fish, meat, vegetables, bone broth — provide these nutrients more reliably than ultra-processed diets.
3. Keep the Neck and Upper Chest Warm
Traditional medicine and modern physiology agree: cold exposure around the neck and upper chest can reduce local blood flow and immune responsiveness, especially to the throat and respiratory tract.
4. Maintain Indoor Humidity
Dry winter air weakens the respiratory mucosa — the body’s first line of defense.
Research shows that maintaining indoor humidity around 40–60%:
A simple humidifier can make a measurable difference.
5. Reduce Inflammatory Load
High sugar intake, chronic stress, dehydration, and ultra-processed foods all impair immune signaling.
Helpful steps include:
A Balanced, Informed Approach
Many physicians still recommend the flu shot, particularly for high-risk individuals. But growing evidence supports a broader view: immune resilience is built daily, not injected once per year.
In seasons where vaccine strain matching is imperfect, strengthening the body’s innate and adaptive immune responses may be just as important — if not more so — than vaccination alone.
This is not about rejecting medicine. It is about using all available tools, including nutrition, sleep, stress regulation, and environmental support, to improve outcomes during a challenging flu season.
References

For years, people with digestive trouble have been told to avoid bread altogether. The common belief is that bread slows digestion, worsens bloating, and contributes to constipation.
New research suggests that belief is only partly true.
According to recently published dietary guidelines from King’s College London, one type of bread stands out as an exception: rye bread.
What the Research Found
In what researchers described as the first evidence-based dietary guidelines for adults with chronic constipation, investigators reviewed data from multiple clinical trials examining diet and bowel function.
Surprisingly, the foods with the strongest evidence for improving constipation were:
In studies comparing rye bread to white bread, only rye bread improved stool frequency and consistency. White bread either had no effect or worsened constipation.
Dr. Roshini Raj, a New York–based gastroenterologist, explained why:
“Rye bread contains both soluble and insoluble fiber. This adds bulk to stool and draws water into the intestine, which improves motility.”
White bread, by contrast, is made from refined flour that has had fiber removed — a known contributor to sluggish bowels.
Why Rye Works Differently Than Other Breads
Rye is structurally different from wheat. It contains:
Rye also provides minerals such as magnesium, zinc, iron, and B vitamins, which support nerve signaling, muscle contraction, and energy metabolism — all relevant to healthy digestion.
According to naturopathic doctor Debra Muth:
“Rye stabilizes blood sugar, feeds the microbiome, and supports motility instead of shutting it down.”
Important Caveat: Not Everyone Tolerates Grains Well
While rye bread can be helpful, it is not appropriate for everyone.
Certain body types and metabolic patterns — including individuals with blood sugar instability, insulin resistance, adrenal stress, or thyroid-dominant metabolism — often do poorly with high carbohydrate intake, even from whole grains.
For these individuals:
In these cases, constipation often responds better to vegetables, healthy fats, hydration, and mineral balance, rather than added grain.
The Key Is Moderation and Individual Fit
For people who tolerate carbohydrates reasonably well, small amounts of whole-grain rye bread can support digestion — especially when paired with:
For others, especially those who feel sluggish, sleepy, or bloated after eating bread, grain reduction or elimination may be necessary, even if rye is technically “healthier.”
How to Choose the Right Rye Bread
If you decide to try rye bread:
As Dr. Raj cautioned, fiber increases should always be gradual, and hydration is essential.
Bottom Line
Rye bread is one of the few breads shown in clinical research to improve constipation — but it is not a universal solution.
Digestive health depends on individual physiology, not one-size-fits-all advice. For some, rye bread can help “keep things moving.” For others, limiting grains altogether may be the better path.
Listening to your body — and adjusting diet accordingly — matters more than following dietary trends.
References

As winter storms sweep across the country, cardiologists are warning that snow shoveling may pose a serious — and often underestimated — risk to heart health, especially for middle-aged and older adults.
Research shows that heavy snow removal can place sudden and extreme strain on the cardiovascular system, sometimes comparable to a medical stress test performed in a hospital setting.
Why Snow Shoveling Is Risky for the Heart
A 2025 Mayo Clinic review found that just 10 minutes of heavy snow shoveling can raise heart rate to nearly 97% of maximum capacity in some individuals. Cold exposure further compounds the risk by:
Together, these factors can sharply increase the risk of heart attack, arrhythmia, or stroke, particularly in people who are not regularly active.
“It’s almost like putting yourself through an unsupervised maximal cardiac stress test,” said Dr. Navjot Kaur Sobti, an interventional cardiologist at Northwell Health.
Is There an Age Cutoff?
There is no official age at which a person is “too old” to shovel snow. However, cardiologists urge extra caution after age 45, especially for:
Dr. John Osborne, a cardiologist and American Heart Association volunteer, notes that many winter cardiac emergencies occur in people who are usually inactive but suddenly attempt heavy exertion.
Cold Weather Adds an Extra Layer of Risk
Cold temperatures alone increase cardiovascular strain. A large study published in the Annals of Internal Medicine (2024) found that cold exposure causes nearly twice as many cardiovascular deaths as heat exposure, with adults over 65 at the highest risk.
Warning Signs Not to Ignore
Stop immediately and seek medical help if any of the following occur while shoveling:
Safer Snow-Removal Tips
If shoveling cannot be avoided, cardiologists recommend:
Snow blowers reduce strain but still elevate heart rate, according to the American Heart Association.
Natural and Supportive Heart-Health Strategies (Complementary Care)
These approaches may help reduce baseline cardiovascular stress during winter months:
1. Hydration and Electrolyte Balance
Cold weather reduces thirst, but dehydration increases blood viscosity and cardiac workload. Adequate fluid intake supports circulation and blood pressure stability.
2. Magnesium Support
Magnesium plays a role in:
Low magnesium levels are associated with hypertension and arrhythmias. Dietary sources include leafy greens, nuts, seeds, and legumes. Supplementation should be discussed with a healthcare provider.
3. Omega-3 Fatty Acids
Omega-3s support:
Found in fatty fish (salmon, sardines) and fish oil supplements.
4. Gentle Conditioning Before Winter
Light, regular activity (walking, resistance bands, mobility exercises) before winter storms improves cardiovascular resilience and reduces shock from sudden exertion.
5. Breathing Control
Slow nasal breathing helps prevent sudden blood-pressure spikes and reduces strain during physical effort.
The Bottom Line
Snow shoveling is not a harmless winter chore — it is a high-intensity cardiovascular event for many people. Age, inactivity, cold exposure, and underlying heart risk factors all combine to increase danger.
If you are unsure about your heart health, delegating snow removal or using mechanical assistance may be the safest choice.
Protecting your heart this winter means respecting its limits — not testing them unexpectedly.
References

Anxiety disorders affect millions of people, and new research is exploring whether nutrition may play a supporting role in brain chemistry related to stress and emotional regulation. A recent analysis suggests that people with certain anxiety disorders may have lower levels of choline in specific brain regions, but experts caution against oversimplifying the findings.
What the Research Found
Researchers at UC Davis Health analyzed data from 25 previously published brain-imaging studies, comparing 370 individuals with anxiety disorders to 342 individuals without anxiety. Using a non-invasive MRI technique called magnetic resonance spectroscopy, they measured brain metabolites rather than blood nutrient levels.
Across the combined studies, individuals with generalized anxiety disorder, panic disorder, and social anxiety disorder showed an average of about 8% lower choline levels in brain regions involved in thinking, emotional regulation, and stress response.¹
Although an 8% difference may seem small, researchers noted that even modest changes in brain chemistry can be meaningful, particularly in regions that help regulate emotional balance.
What Is Choline and Why It Matters
Choline is an essential nutrient, meaning the body produces only small amounts and must obtain the rest from food. It plays an important role in:
Choline is found in foods such as eggs, beef, poultry, fish, soybeans, and dairy products.²
National surveys show that most Americans do not meet recommended choline intake levels, including children and older adults.³
Cause or Consequence?
Importantly, the study does not prove that low choline causes anxiety. The researchers themselves emphasized this point.
One hypothesis is that chronic stress and heightened threat responses in anxiety disorders may increase the brain’s metabolic demand for choline, gradually lowering its levels. In this view, low choline may be a marker of metabolic strain, not the root cause of anxiety.¹
Psychiatrists and nutrition experts interviewed in response to the findings agree that anxiety is multifactorial, involving genetics, life experiences, neurobiology, and environmental stressors—not a single nutrient deficiency.⁴⁻⁶
Should People Take Choline Supplements?
At this stage, experts say no.
While choline is essential, high-dose supplementation can cause side effects, including gastrointestinal distress, low blood pressure, and fishy body odor.⁷ Researchers stressed that it is too early to recommend choline supplements as a treatment for anxiety.
Instead, clinicians suggest reviewing overall diet quality and ensuring adequate intake of brain-supporting nutrients as part of general health guidance, especially for individuals under chronic stress.
Nutrition Is One Piece of a Larger Puzzle
Other nutrients—such as vitamin D, omega-3 fatty acids, magnesium, and B vitamins—have also been linked to mood and anxiety regulation in previous studies.⁸ Nutrition may help support resilience and metabolic balance, but it is not a substitute for evidence-based anxiety treatments, including therapy and, when appropriate, medication.
A balanced diet that includes whole foods like eggs, fish, dairy, vegetables, and healthy fats may support overall brain health, regardless of anxiety status.
Bottom Line
This research highlights a consistent association between anxiety disorders and lower choline levels in key brain regions—but it does not show that choline deficiency causes anxiety or that supplementation is a cure.
The findings open the door for future research into how stress, metabolism, and nutrition interact in the brain, while reinforcing an important principle: mental health is complex, and no single nutrient explains it all.
References

Energy drinks are often marketed as harmless performance boosters, but a recent medical case highlights how excessive consumption can carry serious health risks.
Doctors in the United Kingdom reported that a 50-year-old man suffered a stroke after regularly consuming large amounts of energy drinks, according to a case study published in BMJ Case Reports by clinicians at Nottingham University Hospitals.¹ The man had been generally healthy prior to the event.
What Happened
The patient arrived at the hospital with left-sided weakness, numbness, and poor coordination (ataxia). Brain imaging confirmed an ischemic thalamic stroke, meaning blood flow to a deep brain structure was interrupted.¹
On admission, his blood pressure was markedly elevated. Although it was temporarily controlled during hospitalization, it rose again after discharge—even while he was taking multiple antihypertensive medications.¹
The Energy Drink Connection
During further evaluation, the patient disclosed that he had been consuming eight energy drinks per day, each containing approximately 160 mg of caffeine. That amounts to about 1,280 mg of caffeine daily, far exceeding the commonly cited safe upper limit of 400 mg per day for adults.²
After discontinuing caffeine and energy drink consumption, the patient’s blood pressure normalized, and physicians were able to stop his blood-pressure medications.¹
Why Caffeine Matters
Caffeine is a central nervous system stimulant known to increase blood pressure, heart rate, and vascular tone, especially at high doses. Acute and chronic excessive caffeine intake has been associated with hypertension, arrhythmias, and increased stroke risk in susceptible individuals.³⁻⁵
Energy drinks pose a particular concern because they:
The case authors emphasized that caffeine intake is often not routinely documented during hospital admissions, potentially delaying diagnosis of stimulant-related cardiovascular effects.¹
Expert Perspective
Commenting on the case, medical experts noted that very high caffeine intake can substantially elevate blood pressure, which is a well-established risk factor for ischemic stroke.⁴
Sustained hypertension places stress on cerebral blood vessels and increases the likelihood of vascular injury, particularly in middle-aged and older adults.
Key Takeaways
A Word of Caution
This case does not suggest that occasional energy drink use will cause a stroke. However, it clearly demonstrates that habitual, high-dose consumption can have serious consequences, even in individuals without known cardiovascular disease.
Monitoring caffeine intake, reading labels carefully, and staying within established safety limits are simple steps that may significantly reduce health risks.
References

Hot chocolate is a winter favorite, but recent headlines claim it may weaken bones because of its sugar content. Like many nutrition stories, the truth is more nuanced. Sugar intake does matter for bone health—but hot chocolate itself is not the real culprit. The larger issue is overall diet pattern, not an occasional warm drink.
The Sugar–Bone Connection: What’s Supported
There is solid evidence that chronically high sugar intake can negatively affect bone health.
Research shows that diets high in added sugars can increase the loss of calcium and magnesium through urine, two minerals essential for strong bones. Excess sugar is also linked to systemic inflammation, which can interfere with the bone remodeling process—where old bone is broken down and replaced with new bone.
A 2018 review in Nutrients found that high sugar consumption was associated with reduced bone mineral density and increased osteoporosis risk, particularly when combined with low intake of calcium, magnesium, and vitamin D.¹
Sugary beverages are especially problematic because they deliver large amounts of sugar without fiber, protein, or micronutrients that slow absorption.
Conclusion so far:
Yes—a long-term high-sugar diet can weaken bones, especially if it displaces nutrient-dense foods.
Where the Claim Goes Too Far
The idea that hot chocolate itself weakens bones oversimplifies the issue.
Hot chocolate is often made with milk, which contains calcium, phosphorus, and protein—all beneficial for bone health. A single cup of milk provides about 300 mg of calcium, roughly 25–30% of daily needs for adults.²
The problem arises not from cocoa or milk, but from added sugar, especially in pre-packaged mixes that can contain 20–60 grams of sugar per serving—sometimes more than a candy bar.
However, nutrition science does not support the idea that an occasional high-sugar food causes meaningful bone loss in otherwise healthy individuals. Bone density changes occur over years, not days.
As the National Osteoporosis Foundation notes, overall dietary pattern, physical activity, vitamin D status, and hormone balance play much larger roles than individual foods.³
Cocoa Itself May Be Bone-Friendly
Ironically, unsweetened cocoa may actually support bone health.
Cocoa contains flavanols, plant compounds shown to reduce inflammation and oxidative stress. Some studies suggest flavonoids may help preserve bone density by supporting osteoblast activity (cells that build bone).⁴
A 2020 review in Journal of Nutritional Biochemistry reported that polyphenols from cocoa may have protective effects on bone metabolism when consumed as part of a balanced diet.⁵
The key distinction is unsweetened cocoa vs. sugar-loaded mixes.
What Really Matters for Bone Health
Bone strength depends on several well-established factors:
No single food makes or breaks bone health.
A Practical Takeaway
Bottom Line
The claim that hot chocolate “weakens bones” is partly true but overstated.
Sugar excess is the real issue—not cocoa, not milk, and not the occasional winter drink.
References

As cities grow larger and space becomes tighter, one question keeps coming up: how will we grow fresh food close to where people live? A futuristic project unveiled at Expo 2025 in Osaka, Japan offers one possible answer—a compact, self-contained food dome that works like a miniature ecosystem.
Known as the “Source of Life” dome, this structure shows how food production could move onto rooftops, schools, and apartment buildings instead of relying only on distant farms.
A Mini Ecosystem Under One Roof
At first glance, the dome looks like a small greenhouse. Inside, however, it functions as a fully integrated food system. Fish, plants, microbes, water, and sunlight all work together in a closed loop that produces almost no waste.
The dome is about 21 feet tall and is built around four water zones:
Each zone supports different types of fish. As the fish produce waste, naturally occurring microbes convert that waste into nutrients plants can use. Those nutrients are then pumped upward to stacked plant layers.
Above the water tanks, plants grow in hydroponic tiers, meaning no soil is required. Salt-tolerant greens grow above seawater. Tomatoes and other vegetables thrive above brackish water. Herbs and lettuce grow above freshwater fish. Edible flowers sit at the top, where sunlight is strongest.
The design mirrors how ecosystems transition from ocean to land in nature.
How the System Stays Balanced
The dome uses transparent ETFE panels to let in sunlight while keeping temperatures stable. Water continuously cycles upward to feed plants and then flows back down, cleaned by plant roots and microbes before returning to the fish tanks.
Because everything is reused—water, nutrients, and energy—the system needs very little outside input once it is running. There is no soil depletion, no fertilizer runoff, and no dependence on weather.
Why This Matters for Cities
If systems like this can be scaled, cities could shift food production from large, distant farms to many small local sites. Rooftops, schoolyards, and unused urban spaces could all become food sources.
This approach offers several benefits:
Instead of one massive farm feeding a city, hundreds of small systems could share the load.
Learning From Nature
The dome was designed by researchers from Osaka Metropolitan University and the Tokyo University of Marine Science and Technology. Their goal was not to invent a new process, but to copy how healthy ecosystems already work, especially wetlands where waste from one organism becomes food for another.
By letting biology do most of the work, the system reduces strain on land, water, and energy resources.
What This Could Mean for You
In the future, a food dome like this could sit on top of an apartment building, school, or community center. It could provide herbs, leafy greens, vegetables, and even edible flowers just steps away from where people live.
For people without access to farmland—or even a backyard—this model offers a realistic way to grow clean, fresh food year-round. In emergencies, when transportation is disrupted, these closed-loop systems could keep producing food locally.
Looking Ahead
The Source of Life dome is still a prototype, but it offers a clear glimpse into how food production might change. By combining architecture, aquaculture, and ecology into one compact system, it shows that future cities may not need to choose between density and sustainability.
If adopted widely, food domes could help millions of people reconnect with where their food comes from—without leaving the city.

Sick With a Cold? Why Some “Comfort Foods” Can Actually Make You Feel Worse
When cold and flu season hits, many people instinctively reach for comfort foods. Unfortunately, some of the most common choices can slow recovery, worsen symptoms, and place extra stress on the immune system.
While nutrition alone won’t cure a viral illness, the right foods can support healing, and the wrong ones can make your body work harder than it needs to. Here’s what to avoid when you’re sick — and what to choose instead.
Foods and Drinks to Avoid When You’re Sick
1. Spicy Foods
Spicy meals may seem appealing when taste buds are dulled, but they can backfire.
Capsaicin (the compound that makes foods spicy) can temporarily open nasal passages, which may offer brief relief from congestion. However, it can also:
For some people, mild spice is tolerable. For others, it increases discomfort. When sick, it’s best to prioritize gentle foods that don’t provoke irritation.
2. Alcohol
Alcohol is one of the worst choices during illness.
It negatively affects recovery by:
Even small amounts can slow healing and force your body to fight both the infection and the metabolic stress of alcohol at the same time.
Bottom line: Save alcohol for after you’re well.
3. Fried and Greasy Foods
Fried foods, chips, and greasy comfort meals are hard on the digestive system — especially when you’re already sick.
They can:
Since much of the immune system resides in the gut, digestive stress during illness can interfere with recovery.
4. Sugary Drinks
Sugary sodas, sweet teas, and fruit punches can worsen illness by:
While electrolyte beverages may be helpful in cases of dehydration, most sugary drinks provide little benefit and significant downside during illness.
What to Eat Instead When You’re Sick
When recovering from a cold or flu, focus on foods that are:
Better Choices Include:
These foods provide hydration, nutrients, and energy without taxing digestion.
Hydration Matters
Staying hydrated is critical during illness.
Better options include:
Avoid beverages that increase dehydration or blood sugar spikes.
The Takeaway
When you’re sick, your body needs support — not extra obstacles.
Choosing foods that are simple, nourishing, and anti-inflammatory, while avoiding alcohol, excess sugar, greasy meals, and irritating spices, helps your immune system do its job more efficiently.
Food won’t replace rest or medical care when needed, but smart nutrition choices can shorten recovery time and reduce symptom severity.