




A new study published in Sleep Advances found that adults with high blood pressure improved their readings after only two weeks of doing one simple thing: keeping a consistent bedtime. Participants didn’t sleep longer — they simply went to bed at the same time every night. Reducing their bedtime variability from about 30 minutes to just a few minutes helped restore a healthier overnight blood-pressure rhythm.
Why does this matter? Because the cardiovascular system is tightly linked to the body’s circadian clock. When you keep regular sleep and wake times, hormones such as melatonin and cortisol release in the proper sequence. That rhythm helps set the natural rise and fall of blood pressure throughout the 24-hour cycle.
A consistent schedule also stabilizes the autonomic nervous system, the part of your body that regulates blood pressure, heart rate, digestion, and adrenal output.
Below are several additional natural strategies that work with the body’s regulatory systems to promote healthier blood pressure.
1. Correct Sleep Timing to Support Adrenal and Vagal Balance
Sleep irregularity stresses the adrenal system. A stable bedtime calms cortisol release and allows melatonin to rise naturally. Pair this with:
This strengthens the brain’s “clock genes,” allowing the cardiovascular system to stabilize rather than spike.
2. Hydration and Mineral Balance
Even mild dehydration can raise blood pressure by thickening the blood and increasing vascular resistance. Aim for fluid intake based on weight:
Minerals such as magnesium, potassium, and trace minerals also help smooth vascular tone and support nerve conduction.
3. Chiropractic Alignment and Nervous System Regulation
Structural imbalance — especially in the cervical spine — can influence autonomic output through irritation of sympathetic pathways. Correcting subluxations can help normalize autonomic balance and improve vasodilation, digestion, and adrenal regulation. Many patients with blood-pressure issues benefit from adjusting the upper cervical region, which has strong connections to cardiovascular reflexes.
4. Breathing Techniques to Lower Sympathetic Overdrive
Slow diaphragmatic breathing stimulates the vagus nerve, lowers adrenaline, and can immediately drop systolic readings. Techniques such as:
All help regulate the nervous system that governs blood-vessel tone.
5. Targeted Nutrition for Vascular and Adrenal Support
Nutrients that often support blood pressure balance include:
Blood pressure often improves when inflammation, adrenal strain, and endothelial stress are reduced.
6. Movement That Doesn’t Spike Cortisol
Regular gentle activity — walking, rebounding, stretching, or wobble-seat exercises — improves circulation and helps regulate blood pressure without stressing the adrenals. People with hypertension often do better with steady movement rather than high-intensity exercise late in the evening.
The Takeaway
A consistent bedtime may seem like too small a change to matter, but the body’s circadian system governs hormone release, vascular dilation, and autonomic balance. When sleep timing stabilizes, blood pressure often follows.
Adding hydration, mineral support, chiropractic care, relaxation techniques, and gentle movement creates a powerful combination for cardiovascular wellness — and all of these tools work with the body instead of forcing it.
A major study from the University of New South Wales has confirmed what natural health practitioners have long suspected: social isolation is one of the strongest late-life risk factors for dementia.
Researchers followed 851 adults over age 70 for more than 12 years. Those who were classified as socially frail—meaning low social support, infrequent interaction, limited community involvement, or low purpose—had a 47% higher risk of developing dementia compared to those with healthy social engagement.
Other studies continue to reinforce this finding. Cornell researchers recently demonstrated that consistent, meaningful social relationships slow cellular aging by reducing chronic inflammation—a major driver of cognitive decline.
Neurology and natural healthcare both recognize that the brain depends on three major forms of fuel:
When someone becomes socially isolated, they often experience a drop in mental stimulation, emotional regulation, movement, and even oxygenation to key brain regions—including the frontal and temporal lobes responsible for memory, planning, and language.
This decline in stimulation parallels what chiropractors see every day:
When the nervous system receives less input, the entire body’s function suffers.
Social engagement is essential, but it works best alongside the broader laws of health. A strong brain requires a strong body, and HERE is where natural medicine shines.
Chiropractic adjustments restore proper alignment and motion, which improves the quality of signals traveling between the brain and body. Poor alignment—especially in the cervical spine—reduces blood flow, increases inflammation, and interferes with proprioception, all of which accelerate cognitive decline.
A healthy nervous system supports:
Neurology, biology, and chiropractic philosophy converge on a single point:
The body cannot reach its God-given potential when nerve interference is present.
Natural foods that enhance brain health include:
Patients with inflammation, blood sugar instability, or mineral deficiencies often see improved cognitive function when nutrition is corrected.
Exercise increases brain-derived neurotrophic factor (BDNF), a key molecule for memory and learning. Even simple daily movement—walking, stretching, gentle strength work—dramatically lowers dementia risk.
Chronic stress damages the hippocampus (memory center). Proper rest restores neurological firing patterns and reduces inflammation.
Purpose, gratitude, prayer, and emotional balance strengthen the higher centers of the brain and reduce the physiological stress load. Studies consistently show people with strong spiritual lives experience lower rates of dementia and depression.
When patients combine:
…they give their brain the environment it needs to stay sharp, resilient, and aligned with its full God-given design.
This is why we encourage the simple rule:
“Chiropractic first, drug therapy second, surgery last.”
The safest, most natural approach should always be the first approach.
If you’d like to evaluate your neurological health or explore natural strategies for improving memory, mood, and brain function, we are here to help.

So — yes — there is a scientifically documented recent decline in peanut allergy prevalence in certain groups. It aligns with changing public-health recommendations and feeding practices.
🔎 Why It May Be Happening: Early Allergen Exposure + Immune Tolerance
Researchers believe the following factors may explain the decline:
1. Early Introduction of Peanut in Infancy (“Window of Opportunity”)
2. Reduced Sensitization Through Skin Barrier Protection
3. Improved Public Awareness and Preventive Measures
⚠️ Why We Should Remain Cautious: It’s Still Early, and Not All Allergies Are Covered
Despite encouraging signs, there are several important caveats:
🧭 What This Means
✅ My Best Guess: Why Peanut Allergies Are Declining — But Not Vanishing
Based on the data, the most plausible explanation is:
Because infants are now introduced early to peanuts (during a “tolerance window”), their immune systems are trained to accept peanut proteins. That training, combined with better infant skin care and fewer environmental sensitizers, reduces the rate of new peanut allergies.
That doesn’t guarantee elimination, but it suggests a path toward significantly reducing prevalence — maybe even shifting peanut allergy from “common childhood handicap” back toward “rare sensitivity.”

A new peer-reviewed study published in the Journal of Lipid Research (Deol et al., 2025) is raising important questions about America’s most widely used cooking oil: soybean oil. For decades, discussions about dietary fats have focused on calories and macronutrient ratios. This study takes a different approach by examining how the body metabolizes linoleic acid, the omega-6 fat that makes up a large portion of soybean oil.
And the results should give every health-conscious person pause.
1. What the Study Found
Citation: Deol, S. et al., Journal of Lipid Research, 2025.
Researchers fed mice a diet high in soybean oil and then tracked how their bodies broke down linoleic acid (LA).
Key findings:
a) Linoleic Acid → Oxylipins → Weight Gain
Linoleic acid is metabolized into compounds called oxylipins.
This study found:
In other words, it wasn’t just the calories—it was what the linoleic acid turned into inside the body.
b) Genetically Modified Mice Didn’t Gain the Weight
Researchers used a mouse strain with altered liver gene expression (P2-HNF4α) that reduces the conversion of LA into oxylipins.
When these modified mice ate the same soybean-oil diet, they:
This strongly suggests that the biochemical processing of linoleic acid, not simply “too many calories,” may contribute to obesity.
c) Humans Also Produce These Enzymes
The same oxylipin-producing enzymes exist in humans.
Their activity varies by:
This means some individuals may be far more sensitive to soybean-oil-rich diets than others.
2. What This Means for Human Health
The authors make it clear:
This study does not prove soybean oil causes obesity in humans.
But it does highlight a mechanism that could help explain why obesity rates remain high even when calorie intake isn’t extreme:
This fits well with several other lines of research:
Taken together, this study adds one more piece to a growing puzzle.
3. Which Oils Should You Avoid?
The issue isn’t just soybean oil.
Most seed oils are high in linoleic acid.
Common high-LA oils to minimize:
These oils oxidize easily and contribute to the same oxylipin pathways implicated in metabolic dysfunction.
4. Healthier Oils to Use Instead (Evidence-Supported)
Based on oxidative stability, lower LA content, and metabolic research, the following oils are better options:
1. Extra Virgin Olive Oil (EVOO)
2. Avocado Oil
3. Coconut Oil
4. Butter or Ghee (from grass-fed animals)
5. Beef Tallow
6. Macadamia Nut Oil
5. The Bottom Line
This new study does not say soybean oil automatically causes obesity in every human.
But it does highlight a plausible biochemical pathway:
High–linoleic acid oils → more oxylipins → more inflammation & fat storage.
Given that soybean oil is the single most consumed oil in the United States, this warrants serious attention.
If you want better metabolic control, fewer inflammatory byproducts, and lower oxylipin load, the practical solution is simple:
Replace high-LA seed oils with stable, traditional fats such as olive oil, avocado oil, coconut oil, grass-fed butter/ghee, or beef tallow.
In October 2025, the World Health Organization officially classified Cannabis Hyperemesis Syndrome (CHS) as a distinct medical condition (ICD-10 code: F12.2 and updates). The CDC adopted the classification on October 1, allowing CHS to be diagnosed, tracked, and studied rather than buried inside general gastrointestinal categories.
This update comes at an important moment:
Emergency room visits related to CHS have increased over 650% since 2016 (JAMA Network Open, 2025).
CHS is not rare.
It’s not imaginary.
And it’s not harmless.
1. What the New WHO Code Confirms
Cannabis Hyperemesis Syndrome (CHS) is characterized by:
The NIH describes CHS as “repeated and severe bouts of vomiting in long-term, high-frequency cannabis users.”
(Cleveland Clinic; National Institutes of Health)
The syndrome was once thought to be rare.
Now we know that doctors were simply misdiagnosing it.
2. Why Cases Are Exploding: Ultra-High THC Products
The JAMA (2025) study notes:
According to addiction specialist John Puls, “products over 90% THC” are the common factor in the sharp rise in adolescent CHS cases.
This is not the marijuana of Woodstock or 1970s counterculture.
This is biochemically engineered, industrial-scale THC exposure.
3. The Myth That Marijuana Isn’t Addictive
For decades the public was told:
Those claims are false and outdated.
According to the National Institute on Drug Abuse (NIDA):
About 30% of cannabis users develop Cannabis Use Disorder (CUD).
(NIDA, 2022)
And adolescents are 4–7 times more likely to develop addiction compared to adults.
The proof that marijuana is addictive is simple:
Marijuana addiction is real.
And it is accelerating.
4. The Adolescent Brain: Why Teens Are at Highest Risk
The human brain does not finish developing until ~25 years old.
During adolescence the prefrontal cortex—responsible for judgment, impulse control, emotional regulation, and planning—is still developing.
High-THC cannabis interferes with:
Research published in The Lancet Psychiatry (2019) found:
The adolescent brain is simply not built to tolerate industrial-strength THC.
5. The Neurological and Psychiatric Risks No One Mentioned
Researchers now link high-potency THC with:
A 2022 NIH-funded study showed:
High-potency cannabis users had a 3–5× increased risk of psychosis
compared to non-users.
This is not a culture war talking point.
This is peer-reviewed neuroscience.
6. Marijuana and Lung Damage: The “Cleaner Than Cigarettes” Myth
Another myth that needs dismantling:
Smoking marijuana is not harmless to the lungs.
The American Lung Association states:
Marijuana smoke contains many of the same toxins, irritants, and carcinogens as tobacco smoke.
Peer-reviewed studies show marijuana smoke is associated with:
A 2022 Radiology study showed:
Again, the idea that marijuana is “safe” comes from the 1970s culture, not modern toxicology.
7. What CHS Tells Us: The Drug Is Changing, Not the Human Body
CHS does not happen because:
CHS is tied directly to:
The WHO adding CHS to its diagnostic manual is not a trivial move.
It is a recognition that marijuana—specifically modern high-potency cannabis—is biochemically different from historic forms of the drug.
8. Why This Matters for Parents, Teens, and Policy Makers
Parents were told:
But today’s teens are using:
And they are paying the neurological price.
Emergency rooms now report:
The data are no longer deniable.
9. Bottom Line
The WHO’s new classification did not create a new disorder.
It simply acknowledged what emergency physicians have been seeing for a decade:
The public narrative of “safe, natural, harmless weed” has not kept pace with the science.
The drug changed.
The potency changed.
The delivery systems changed.
And the health consequences changed as well.
When a substance sends ER visits up 650% in less than 10 years, it’s time for honest public discussion—not outdated cultural slogans.

Pumpkin usually gets attention only around the holidays, but its nutritional value extends far beyond pies and lattes. Whether you use fresh pumpkin, canned purée, or pumpkin seeds, this humble food offers meaningful health benefits—especially for the heart, gut, immune system, and metabolic balance.
Here’s a clearer and more complete look than what you often see in mainstream articles.
1. Heart Health and Potassium Balance
One cup of plain organic pumpkin purée delivers about 500 mg of potassium, which helps balance sodium and maintain healthy blood pressure.
Many patients are potassium-deficient without realizing it, and adding pumpkin to meals is an easy way to close that gap.
2. Fiber for Digestion, Satiety, and Blood Sugar Control
Pumpkin contains both soluble and insoluble fiber.
Soluble fiber slows glucose absorption, supports short-chain fatty acid production, and helps repair the gut lining—useful for patients with IBS, leaky gut tendencies, or post-antibiotic recovery.
Fiber also creates a feeling of fullness, which helps regulate appetite naturally.
3. Antioxidants and Carotenoids—With an Important Clarification
Pumpkin is rich in beta-carotene and other carotenoids that fight oxidative stress. These compounds support eye health and reduce inflammation.
But remember: carotenoids must be converted into active vitamin A.
This conversion requires healthy thyroid function, adequate zinc, iron, and good fat metabolism. Many adults convert poorly, so pumpkin should be viewed as supportive, not a primary vitamin A source.
(Clinically, this matters because we include vitamin A in many protocols when indicated.)
4. Pumpkin Seeds: Minerals, Protein, and Metabolic Support
Pumpkin seeds (pepitas) are nutrient powerhouses. They offer:
For best benefit, choose raw or lightly roasted seeds to avoid oxidized oils.
5. Easy Ways to Add Pumpkin to Your Diet
When buying canned pumpkin, check the label:
Choose cans that say “organic pumpkin” only—avoid pumpkin pie mix because it contains added sugar.
Final Thoughts
Pumpkin is far more than a seasonal ingredient. It supports heart health, gut repair, metabolic wellness, immune function, and healthy inflammatory balance. Combined with the mineral-rich benefits of pumpkin seeds, it’s one of the most versatile foods you can add to your daily routine.

Short intro:
GLP-1 agonists like Ozempic, Wegovy, Mounjaro, and Zepbound are marketed as “miracle” weight-loss drugs. But once you sift through the data—not the ads—you see a clear pattern: these drugs override your body’s regulatory networks, and the body eventually pushes back. Hard. And financially, these drugs lock people into a lifelong dependency that few can afford.
1. What These Drugs Actually Do (Mechanistically)
GLP-1 agonists artificially elevate a gut hormone that slows stomach emptying, suppresses appetite, and spikes insulin output.
They do not fix:
They simply overpower normal signaling.
2. Short-Term Benefits—With Significant Costs
Common adverse effects
• Persistent nausea, vomiting, diarrhea (FDA)
• Gallbladder issues & gallstones (JAMA, 2023)
• Up to 40% of weight lost is muscle mass (Nature Medicine, 2024)
• Emotional blunting and anhedonia (J Clin Psychopharm, 2023)
• Slowed metabolism that persists after discontinuation
3. Long-Term Research: A System That Fights Back
The long-term data is the real warning sign:
• Weight regain is the rule, with most patients regaining two-thirds within a year of stopping (NEJM STEP-1 Extension, 2022).
• Resting metabolic rate stays low, long after discontinuation.
• Pancreatic stress markers rise (Gastroenterology, 2023).
• Intestinal enlargement documented in animal models (Cell Reports, 2024).
When you override a feedback loop, it eventually destabilizes.
4. The Financial Trap: “Take It for Life”
This is rarely discussed openly—because it’s the biggest liability.
Average cost without insurance:
That’s $12,000–$18,000 a year—often indefinitely.
And here’s the kicker:
Once you stop the drug, the weight almost always returns.
This creates a pharmaceutical annuity model: pay forever, or gain the weight back.
For many patients, the cost of the drug becomes larger than the cost of housing, groceries, or even their car.
5. You Can’t Out-Hack a Regulatory Network
Hormonal systems (leptin, insulin, adrenal rhythm, thyroid, ghrelin) operate as an integrated network.
When one node is forcibly overridden:
• Metabolism drops
• Hunger signals rebound
• Muscle breaks down
• The body “defends” its weight
When you trick the body, the body wins in the long run.
Final Thought
True metabolic recovery comes from restoring regulatory balance—not overpowering it with a drug you’ll need forever. Strengthen leptin signaling, repair insulin handling, regulate adrenals/thyroid, correct nutrient deficiencies… and the body does what it was designed to do naturally.
In the world of chiropractic care, one of the foundational principles we hold is the idea of innate intelligence. Think of innate intelligence as your body’s built-in, God-given wisdom—an internal guiding force that helps maintain balance, heal injuries, and keep you thriving.
Now, how does this innate intelligence actually work in day-to-day life? It flows through your nervous system. Your brain and spinal cord are the main highways for this intelligence, sending signals that help coordinate everything from your heartbeat to your immune responses. When your spine is aligned, those signals travel freely. But when you have misalignments—what we call subluxations—that communication can get disrupted.
In other words, by adjusting the spine and keeping your nervous system in top shape, we’re not just working on bones—we’re supporting your body’s natural ability to heal and function as it was designed to. It’s a simple yet powerful idea: when you remove interference, you let innate intelligence do its job.
So if you’ve ever wondered why chiropractic care focuses so much on the spine, it’s because we see it as the gateway to your body’s own healing power. And that’s the beauty of innate intelligence—it’s already within you, just waiting to be unlocked.
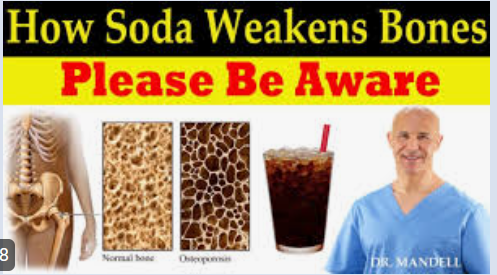
Most people think of soft drinks as harmless treats, but the science paints a very different picture. Soda—whether regular or diet—quietly damages bone health for years before any symptoms appear. The imbalance these drinks create in your mineral chemistry can lead to weak bones, premature fractures, poor healing, and chronic joint and muscle problems.
A recent large-scale study shows that daily soda drinkers have nearly five times the fracture risk compared to non-drinkers. Even those who drink only one to two sodas per week have a measurable increase in fracture likelihood.
If you want strong bones as you age, eliminating soft drinks is one of the most important decisions you can make.
Daily Soda Intake Raises Fracture Risk by Nearly 5-Fold
A major study published in Nutrients followed 17,383 adults over five years. The findings were clear:
Key Findings
This means the soda itself—not lifestyle—is driving the problem.
How Soft Drinks Damage Bone Health
Soft drinks harm your bones through multiple mechanisms, not just “bad nutrition.”
1. Phosphoric Acid Disrupts Mineral Balance
Sodas—especially colas—contain phosphoric acid, which throws off your body’s calcium-to-phosphorus ratio. When phosphorus rises, your body must pull calcium out of your bones to rebalance the chemistry.
This leads directly to:
Even people who consume enough dietary calcium suffer bone loss if they drink soda.
2. Soda Replaces Bone-Building Foods
Soft drink users drink:
This further amplifies the mineral deficit.
3. Soda Fuels Obesity, Which Increases Fracture Risk
Soft drinks contribute to:
Obesity shifts how forces travel through the skeleton, increasing fracture risk—especially in hips, shoulders, and upper limbs.
Diet Soda Is Even Worse for Bones
A study in the International Journal of Clinical Biochemistry and Research compared three groups:
The diet soda group had:
This held true even when all groups ate identical diets.
Diet soda is not a safe alternative. It causes more bone loss than regular soda.
Why Diet Soda Damages Bones
Diet sodas contain:
This biochemical mixture interferes with:
When vitamin D activation drops, your body cannot absorb calcium even from a good diet. Your bones become the backup supply—and they pay the price.
How to Reverse the Damage
Bone loss can be slowed and often reversed—but only if the source of the problem is removed.
1. Eliminate All Sodas Completely
Cut out:
Every version interferes with bone health.
Replace them with:
2. Rebuild Your Mineral Base
The following foods help restore bone density:
Vitamin K2 is essential for guiding calcium into your bones and keeping it out of your arteries.
3. Restore Vitamin D Through Safe Sun Exposure
Vitamin D is critical for bone metabolism.
For optimal vitamin D:
When vitamin D levels normalize, calcium absorption and bone remodeling improve dramatically.
4. Strengthen Bones Through Movement
Bone responds to stress by rebuilding itself. The most effective strategies include:
FAQs About Soda and Bone Damage
Q: How quickly can soda cause bone loss?
The damage is slow and silent. But studies show measurable fracture risk within five years.
Q: Are diet sodas safer?
No. Diet sodas are more damaging to bone density than regular soda.
Q: Can bone damage be reversed?
Yes, but only by eliminating sodas and rebuilding mineral reserves with proper nutrition, sunlight, and exercise.
Q: What symptoms indicate soda-related mineral imbalance?
The Bottom Line
Soda weakens your bones, disrupts mineral metabolism, lowers vitamin D, and accelerates bone breakdown—even when your diet is otherwise good. Both regular and diet versions create a persistent biochemical environment that erodes your skeletal strength.
Protect your bones now so you’re not paying for soda with fractures later in life.

In the world of nutritional therapy, you quickly learn a hard truth: drug companies can say almost anything once a product is approved, while nutritional companies can barely say anything at all — even when the evidence is solid.
The imbalance is so extreme that, at times, the federal government has treated scientific information itself as a controlled substance.
As strange as that sounds, it has happened — and the 1992 armed raid on a nutrition clinic is one of the clearest examples.
The Day the FDA Treated a Nutritional Study Like a Criminal Substance
On May 6, 1992, the offices of Dr. Jonathan Wright, a Harvard-educated physician associated with the Life Extension Foundation, were stormed by FDA agents and local law enforcement.
Not because the clinic harmed patients.
Not because of mislabeled supplements.
Not because of contaminated stock.
The “crime” was distributing a published scientific study on folic acid.
The study described how folic acid supports normal neural-tube development in embryos — research that today is universally accepted and recommended by every OB/GYN in America.
But at the time, because the Life Extension Foundation also sold folic acid supplements, the FDA claimed that sending out a peer-reviewed study amounted to an illegal “disease claim.”
The result was surreal:
This episode became a defining moment in the movement to reform supplement laws and protect freedom of health information.
Why Sharing Science is Treated as a Crime in the Supplement Industry
Under the Dietary Supplement Health and Education Act (DSHEA), nutritional companies are legally forbidden from claiming that:
can treat, cure, diagnose, or prevent any specific disease.
It does not matter if:
If a supplement company even quotes a medical journal in a way the FDA interprets as implying disease treatment, it becomes a regulatory offense.
Drug companies, by contrast, can advertise directly to the public and make sweeping statements of efficacy — even when the drug barely outperforms a placebo.
This is the core constitutional issue: truthful scientific information should not be illegal speech.
The Placebo Problem: When Approved Drugs Barely Work Better Than Sugar Pills
The irony deepens when you look at how many pharmaceuticals reach the market with very small advantages over placebo.
In some drug classes — psychiatric medications especially — the difference between the drug and placebo is sometimes so small that only statistical gymnastics reveal significance.
Some examples:
And yet, once a drug has its approval stamp, the marketing machine rolls ahead full force.
Commercials proclaim:
even when the improvement is statistically detectable but practically small.
Nutritional companies, meanwhile, cannot legally say:
unless phrased through extremely narrow, FDA-approved structure-function language.
The irony is hard to miss.
A Regulatory Double Standard With Real Consequences
The end result is a system where:
1. Pharmaceutical companies can advertise aggressively
—even when the drug only modestly outperforms placebo.
2. Nutritional companies must censor scientific truth
—even when the evidence is peer-reviewed, well-established, or part of standard medical practice.
3. Practitioners who rely on nutritional science must walk a legal tightrope
to avoid “unapproved claims,” even when their advice is safer than available drugs.
4. Consumers end up hearing only one side
because the other side is legally prohibited from speaking.
The 1992 raid was not an isolated mistake but a symptom of a larger problem: a regulatory philosophy that treats natural health information as a threat rather than an asset.
The Real Issue: Who Controls Health Knowledge?
This isn’t ultimately about vitamins vs. drugs.
It’s about whether free citizens have the right to:
When government agencies treat information as contraband, it raises profound questions about free speech — especially when the information is true, peer-reviewed, and harmless.
The Life Extension raid was a reminder that the struggle is not merely about supplements; it's about who owns scientific knowledge — the public, or the state?
Conclusion: Toward an Honest Conversation About Healing
If a drug barely beats placebo, consumers deserve to know that.
If a nutrient has proven benefits, companies deserve the right to state that.
If published science exists, citizens deserve the right to read it without gatekeepers.
The purpose of health regulation should be to protect consumers from harm — not to protect one industry’s profits, nor to suppress truthful speech.
The goal is simple:
The future of healthcare depends on something deeper than regulation — it depends on trust, and trust can only exist where truth is allowed to be spoken.
Courtesy of:
John H. Keefe III, D.C.
(918) 663-1111
WELLNESS: HOW SLOW BREATHING ALTERS BRAIN CIRCUITS TO CRUSH ANXIETY Research has identified a brain circuit involving the anterior cingulate cortex, pons and medulla that links slow breathing to reduced anxiety. Activating this circuit in mice led to slower breathing and decreased anxiety, while shutting it off increased stress and breathing rates. The discovery of this brain circuit provides a neurological basis for practices like yoga and mindfulness. Another study found that torso stiffness, a common stress response, limits venous return and cardiac output, exacerbating anxiety symptoms. Aerobic exercise and proper breathing reduce torso stiffness, improve circulation and prevent negative effects on your cardiopulmonary system. Understanding the biomechanics of how the body responds to anxiety is helpful for developing holistic treatment strategies. Techniques that promote muscle relaxation and enhance circulation, such as aerobic exercise and controlled breathing, are useful for anxiety treatment plans. By addressing both the neurological and physical aspects of anxiety, it allows for a more comprehensive approach to managing anxiety. This includes integrating breathing techniques and physical exercise to alleviate symptoms and promote overall well-being. Front. Public Health, October 7, 2024, Sec. Public Mental Health, Volume 12--Neuroscience News, November 19, 2024--Nature Neuroscience November 19, 2024, 27, 2455-2465--Front Sports Act Living. 2024 Nov 1;6:1487862
CHIROPRACTIC: CHIROPRACTIC CARE DURING PREGNANCY can help maintain pelvic alignment, reduce back and joint pain, and support proper nerve function, which may lead to shorter labor and delivery times. It is a safe, drug-free option to relieve common discomforts and promote overall wellness. Diet plays a vital role in a healthy pregnancy by providing nutrient-dense, whole foods rich in protein, healthy fats, and complex carbohydrates to support fetal growth, brain development, and maternal energy. Avoiding processed foods and excessive sugars helps prevent issues like gestational diabetes. Nutritional therapy further supports pregnancy by addressing individual deficiencies in key nutrients like folate, iron, magnesium, calcium, and B vitamins, which are crucial for the baby’s development and the mother’s well-being. It also enhances immune function, reduces fatigue, and helps regulate hormones and blood sugar for a healthier, more comfortable pregnancy experience. Borggren, C. L. (2007). "Pregnancy and chiropractic: a narrative review of the literature." Journal of Chiropractic Medicine, 6(2), 70–74. https://doi.org/10.1016/j.jcme.2007.02.011--Koletzko, B. et al. (2007). "Dietary fat intakes for pregnant and lactating women." British Journal of Nutrition, 98(5), 873–877. https://doi.org/10.1017/S000711450783296X--King, J. C. (2000). "Physiological and metabolic adaptations to pregnancy." American Journal of Clinical Nutrition, 71(5), 1218S–1225S. https://doi.org/10.1093/ajcn/71.5.1218s
FUNNY BONES: FUNNY INSURANCE CLAIMS: "I bumped into a lamp-post which was obscured by human beings."@@"The accident was caused by me waving to the man I hit last week."@@"I knocked over a man; he admitted it was his fault for he had been knocked down before."@@ A client of mine claimed he broke his arm cycling to work when taking a shortcut through a farm: "I came around a corner and was run off the road by a herd of guinea pigs..." (The farmer verified the claimant's story. Apparently the farmer's daughters' pets had escaped and multiplied into plague proportions.)@@ "I was unable to stop in time and my car crashed into the other vehicle. The driver and passengers then left immediately for a vacation with injuries."

Muscle spasms and twitches are common signs that something in the body’s balance is off. While most people think of them as “just tight muscles,” they’re often the body’s way of signaling deeper issues involving nervous system stress, mineral imbalance, dehydration, or joint misalignment.
1. The Role of Muscle Imbalance
When muscles on one side of a joint become tight or overactive, opposing muscles weaken or lose tone. This imbalance can pull the spine or joints out of their ideal alignment, increasing tension on nerves and blood vessels. Over time, this can trigger pain, twitching, or even referred sensations elsewhere in the body.
Chiropractic adjustments help restore proper joint motion and nerve communication, which allows the muscle system to normalize again. Once nerve interference is reduced, muscles can relax and strengthen more evenly.
2. Fluid and Electrolyte Balance
Muscle tissue depends on precise hydration and mineral balance for proper contraction and relaxation.
3. pH and Mineral Dynamics
A body that’s overly acidic (low pH) can leach minerals such as calcium and magnesium from tissues, increasing the likelihood of cramping and fatigue. Supporting pH balance through a diet rich in vegetables, greens, and mineral-based supplements helps buffer acidity and maintain the muscle’s ability to relax. Chiropractic care complements this by improving circulation and nutrient delivery to those tissues.
4. Nutritional Support
Specific nutrients play key roles in muscular stability:
At Keefe Clinic, we often recommend individualized nutritional programs based on testing, ensuring that supplementation matches each patient’s biochemical needs.
5. Stretching and Postural Correction
Once the nervous system and chemistry are balanced, stretching and posture-based exercises help retrain muscle memory. Gentle daily stretching, coupled with chiropractic adjustments, restores normal range of motion and prevents recurring tightness.
The Takeaway
Muscle spasms and twitches are not random—they’re messages. The key to lasting relief lies in addressing the underlying imbalances in alignment, minerals, fluids, and pH. Through chiropractic care, nutritional support, and guided exercise, the body can restore balance and regain comfortable, natural motion.
For evaluation or questions, contact:
Keefe Clinic
5016 S. 79th E. Avenue, Tulsa, OK
📞 (918) 663-1111 | 📠 (918) 663-2129

How Chiropractic, Nutrition, and Lifestyle Shape Brain Health and Mental Clarity
The mind and body are inseparable. Every thought, emotion, and memory is built upon the communication network of the nervous system—and that network depends on a healthy spine, balanced chemistry, and a
Naturally supportive environment. Building a strong mind begins with maintaining the integrity of the system that feeds it.
1. The Chiropractic Connection: Restoring Communication Between Brain and Body
Your nervous system is the electrical grid of your body, and the spine is its main conduit. When vertebrae lose proper alignment, they can interfere with the flow of nerve impulses between the brain and every organ, gland, and tissue.
Studies have shown that spinal adjustments can influence brain and nervous system activity. For example, one study found that a single session of spinal manipulation therapy (SMT) led to increased activity in the right parahippocampal gyrus, right dorsolateral prefrontal cortex, and left precuneus in patients with chronic low back pain. Frontiers
Another review concluded: “In the past two decades, research has demonstrated that chiropractic spinal adjustment has a neural plastic effect on the central nervous system (CNS).” Frontiers
These findings suggest chiropractic care may improve nervous system communication, thereby supporting mental focus, memory, and resilience.
2. Nutrition for Mental Focus and Memory
The brain is roughly 60 % fat, and every thought requires energy. Nutritional therapy provides the raw materials your brain needs to function efficiently. The right nutrients can boost neurotransmitter balance, improve oxygen delivery, and reduce inflammation—three pillars of healthy cognition.
Key nutrients for brain health:
Foods that challenge mental clarity:
Let food be information: nourished brain, clearer thinking.
3. Exercising the Mind
Just like muscles, the brain thrives on challenge. Activities such as crossword puzzles, memory games, learning a new skill, or playing musical instruments strengthen neural pathways and create new ones—this is neuroplasticity in action. Even five minutes per day of mental stretching (solving a riddle, reading a complex article, learning a new word) builds resilience in the brain’s executive functions.
4. The Power of Movement and Fresh Air
Physical movement increases blood flow to the brain, delivering oxygen and nutrients vital for alertness and memory. Simple walking—especially outdoors—boosts mood-enhancing neurotransmitters like serotonin and dopamine.
Additionally, spending time in fresh air supports vitamin D production and reduces indoor toxin exposure. In contrast, too much time indoors breathing recycled air and under artificial lighting can suppress energy, disrupt sleep rhythms, and dull concentration.
5. Protecting Your Brain from Environmental Toxins
Indoor environments are often loaded with volatile organic compounds (VOCs), mold spores, cleaning chemicals, and electromagnetic stress—all of which can burden the nervous system. Brain fog, fatigue, irritability often have an environmental component.
Simple steps:
6. The Integrated Approach
True mental health comes from integration—aligning structure (spine), chemistry (nutrition), and environment (lifestyle). Chiropractic adjustments keep the nervous system clear; nutritional therapy supplies the brain’s raw materials; movement, oxygen, and mental exercise keep the circuitry active and strong.
The mind isn’t just a by-product of the brain—it’s a living reflection of how well your entire system communicates and adapts. By nurturing that system naturally, you don’t just protect your mind—you build it.
Vienna, Austria — April 13, 2025 — A groundbreaking study presented today at the ESCMID Global 2025 conference in Vienna has revealed a devastating statistic: over 3 million children worldwide died in 2022 from infections linked to antimicrobial resistance (AMR).
The findings spotlight AMR as one of the most urgent global health crises of our time—particularly for children in South-East Asia and Africa, where the burden is highest.
A Mounting Global Threat
The study found that in 2022 alone, 752,000 children in South-East Asia and 659,000 in Africa died of AMR-related complications, with more than 1.5 million additional deaths recorded across other regions. Many of these fatalities were linked to the overuse of so-called Watch and Reserve antibiotics—powerful drugs meant to be used sparingly.
Professor Joseph Harwell, co-author of the study and Senior Clinical Director at the Clinton Health Access Initiative (CHAI), warned of dire consequences if trends continue unchecked:
“While the rise in use of Watch and Reserve antibiotics may be necessary to combat resistant infections, the sharp increase poses serious long-term risks. If bacteria develop resistance to these drugs, there will be few, if any, alternatives left to treat multidrug-resistant infections.”
Why Children Are at Greater Risk
Children remain one of the most vulnerable populations affected by AMR, yet they are often neglected in global health initiatives. CHAI, as a founding member of the Global Accelerator for Paediatric Formulations (GAP-f) with the World Health Organization (WHO), continues to advocate for greater investment in pediatric medicine development and access.
The crisis is worsened in low- and middle-income countries by a combination of overcrowded hospitals, inadequate sanitation, limited diagnostics, and the overuse or misuse of antibiotics—often prescribed without confirmation of bacterial infection.
Between 2019 and 2021, the study found the use of Watch antibiotics increased by 160% in South-East Asia and 126% in Africa, while Reserve antibiotics use rose by 45% and 125% in the same regions, respectively.
Urgent Call for Coordinated Global Action
Experts emphasize that addressing AMR requires a “One Health” approach, connecting human, animal, and environmental health systems. Professor Harwell urged policymakers to adopt stronger, evidence-based stewardship:
“We need cost-effective systems that inform treatment guidelines and measure intervention impact. Policymakers must mandate hospital-based antimicrobial stewardship programs in all pediatric healthcare facilities, and improve age-specific classifications to better track resistance patterns among children.”
Countries such as Côte d’Ivoire, Ghana, Kenya, Malawi, South Africa, and Tanzania have begun implementing surveillance systems and national AMR policies—but the study concludes that far greater global coordination is needed to prevent future generations from facing a post-antibiotic era.
Natural Ways to Strengthen the Immune System and Combat Infection
While the global community works to slow antibiotic resistance, individuals can take meaningful steps to support natural immunity and help the body resist infections more effectively.
1. Optimize Nutritional Defenses
A diet rich in antioxidants, vitamins, and minerals supports every phase of immune function. Key nutrients include:
2. Maintain Gut Health
Approximately 70% of the immune system is located in the gut. Probiotics (like Lactobacillus and Bifidobacterium strains) and prebiotic fibers (found in onions, leeks, and bananas) strengthen gut integrity and limit harmful bacterial growth.
3. Strengthen Natural Barriers
Regular hydration, nasal saline rinses, and adequate sleep maintain healthy mucous membranes—the body’s first line of defense against pathogens.
4. Reduce Chronic Stress
Prolonged stress suppresses immune function by elevating cortisol. Prayer, breathing exercises, moderate exercise, and quiet reflection all support balanced immune regulation.
5. Support with Herbal and Nutritional Adjuncts
Research supports immune-modulating botanicals such as echinacea, elderberry, astragalus, garlic extract, and andrographis for their antiviral and antibacterial effects. Always use them under professional supervision.
6. Chiropractic and Nervous System Support
Since immune response is closely regulated by the nervous system, maintaining proper spinal alignment and nerve function can help optimize immune coordination and recovery.
Takeaway
Antimicrobial resistance is a global crisis, but personal health resilience starts with strengthening the body’s innate defenses. Proper nutrition, rest, and natural support not only reduce infection severity but may also decrease the need for unnecessary antibiotics—helping preserve their effectiveness for those who truly need them.
What the study actually did
• A Japanese team synthesized 12 “hybrid” vitamin-K molecules by grafting a retinoic-acid side chain onto vitamin K (MK-4). In cell studies, several of these analogues drove neural progenitors to become neurons at ~3× the potency of natural MK-4. In mice, lead compounds crossed the blood–brain barrier and boosted brain MK-4 levels. Shibaura Institute of Technology+1
Why people are talking about it
• Fox News and other outlets highlighted the “reversing brain damage” angle, but the primary sources frame these as candidate regenerative agents that now need animal efficacy and safety testing, then clinical trials. Fox News+2EurekAlert!+2
Bottom line for practice (for now)
• These are lab-made analogues, not off-the-shelf vitamins. They’re not ready for patient use. Retinoids can have real toxicities, and high-dose vitamin K can interact with anticoagulants—don’t extrapolate to supplementation. Watch for: (1) Alzheimer’s mouse-model efficacy (behavior + pathology), (2) toxicity/PK studies, and (3) phase-1 trials or trial registrations. Shibaura Institute of Technology
But here’s how you can use these vitamins to stay ahead of health problems. And we can evaluate your status for these important nutrients. Call 918-663-1111.
Vitamin A—especially in its active metabolite retinoic acid (RA)—plays a deep and multifaceted role in the health, repair, and function of neural tissue. Here’s a detailed breakdown:
1. Brain Development and Neural Differentiation
During embryonic development, retinoic acid acts as a morphogen—a signaling molecule that tells immature cells what type of neuron to become and where to go.
2. Synaptic Plasticity and Memory Formation
In the adult brain, vitamin A derivatives modulate genes involved in synaptic plasticity, which underlies learning and memory.
3. Neuroprotection and Anti-inflammatory Effects
Vitamin A helps stabilize and repair neural tissue through several mechanisms:
4. Retinoic Acid and Neurogenesis
In the adult hippocampus—a region central to memory—retinoic acid stimulates the formation of new neurons (neurogenesis).
This is one reason researchers combine retinoic acid with other agents, such as vitamin K analogues, in regenerative experiments: it encourages both cell growth and proper differentiation.
5. Clinical Implications
In short, vitamin A (via retinoic acid) acts as a gene-level regulator for neuron formation, repair, and communication—essentially a molecular “architect” for the brain. It doesn’t merely protect nerve tissue; it helps build and rewire it.
Vitamin K₂ compounds have longer-chain side groups that change where they act and how long they stay in circulation.
| Goal | Best-supported form | Typical dose range |
| General cardiovascular & bone health | K₂ (MK-7) | 90–200 µg/day |
| Osteoporosis therapy (clinical strength) | K₂ (MK-4) | 15–45 mg/day (used in Japan under supervision) |
| Basic clotting support | K₁ | met through vegetables |
Vitamin K works closely with vitamin D₃ and vitamin A/retinoids—they coordinate calcium metabolism and gene regulation. Many practitioners pair MK-7 (or MK-4) with D₃ for better bone and vascular outcomes.
Summary:
For most healthy adults, vitamin K₂ (MK-7) is the most practical and well-studied form for long-term cardiovascular and skeletal benefits. MK-4 may have additional tissue-specific and neurological advantages, but it requires higher, supervised dosing.
Week of: Monday Oct. 13, 2025
Courtesy of:
John H. Keefe III, D.C.
(918) 663-1111
IN THE NEWS: The Honest Truth About Vaccine Effectiveness When a vaccine is said to be “95% effective,” it sounds like 95% of people are protected—but that’s not exactly how those numbers are measured. How It’s Calculated Effectiveness comes from comparing infection rates in vaccinated vs. unvaccinated groups: If 2% of unvaccinated people catch a disease and only 0.1% of vaccinated people do, the vaccine is said to be 95% effective. That’s a statistical comparison, not a direct measure of immunity. What’s Often Overlooked -Natural immunity: Many “unvaccinated” participants already have protection from prior infection.-Population bias: Differences in age, health, or exposure risk affect results.-Waning immunity: Effectiveness drops over time—sometimes within a few years. -Case definitions & testing rates: How “infection” is defined or tested varies widely. -Behavioral factors: Those who vaccinate often differ in habits and exposure. What It Really Means Vaccine effectiveness reflects short-term relative risk reduction, not absolute or lifelong protection. It’s useful for public health planning but limited as a measure of true biological immunity. Honest science means acknowledging those limits and communicating them clearly. CDC: Pertussis Vaccine Effectiveness and Duration of Protection — cdc.gov/vaccines/vpd/dtap-tdap-td--Witt MA et al., Clin Infect Dis, 2012 – Waning immunity in California outbreaks.--Sheridan SL et al., PLOS ONE, 2014 – Acellular pertussis vaccine efficacy over time.--Domenech de Cellès M et al., PLoS Pathog, 2016 – Natural immune boosting and pertussis dynamics.--Klein NP et al., Pediatrics, 2019 – Effectiveness and duration of DTaP vaccine protection.
CHIROPRACTIC MONTH: American Chiropractic Association (ACA) has announced a national health care observance--October is
National Chiropractic Month
DO YOU KNOW SOMEONE WITH A HEALTH PROBLEM OR IN PAIN? INVITE YOUR FAMILY OR FRIENDS TO THE PARTY Who do you know who is hurting? Who do you know that you have been trying to get started at Keefe Clinic? Now is the time to get your spouse or child started on the road to good health.
Complimentary DIAGNOSTIC WORK UP DURING OCTOBER Complimentary initial exam and one X-ray. Tell someone today
WELLNESS: Get Ready for Winter: Strengthen Your Immunity Naturally As the temperatures drop and indoor heating begins, your body faces a double challenge—cold, damp outdoor air and dry, recycled indoor air. Both can stress the immune system and make it easier for seasonal illnesses to take hold. Now is the perfect time to support your health through nutrition, hydration, and chiropractic care. Hydration: Your First Line of Defense Dry indoor air and heated environments draw moisture from your body. Even mild dehydration reduces circulation, slows lymphatic flow, and weakens the immune response. Use this simple hydration formula: Half your body weight (in pounds) = ounces of water daily. For example, a 160-lb person should drink about 80 ounces daily. For optimal flushing, aim for up to 80% of that amount minimum each day. If you’re drinking coffee or tea, add extra water to offset their dehydrating effects. Proper hydration also keeps mucous membranes moist—your natural barrier against viruses and bacteria. Feed Your Immunity A nutrient-dense diet helps your immune cells perform at their best. Protect Your Neck and Maintain Healthy Indoor Air Chilly drafts across the neck and upper back can tighten muscles, reduce circulation, and make you more susceptible to sinus and upper respiratory problems. Keep your neck warm when outdoors, especially in wind or damp conditions. Indoor humidity should be maintained between 40–60% to keep mucous membranes and nasal passages from drying out. Use a humidifier if your home air feels overly dry. The Role of Chiropractic Care Regular chiropractic adjustments help your nervous system function optimally.. Check Your Immune Readiness with Vega Testing Each person’s immune system has unique strengths and weaknesses. Vega testing can help evaluate your immune balance, detect stress points, and identify nutritional needs before symptoms appear. It’s an effective way to make sure your body is ready for the changing season. Doctor’s Tip “True prevention begins before the first frost. Stay hydrated, eat clean, keep your spine aligned, and guard against cold drafts. Your immune system will thank you.”
FUNNY BONE: When a cold, a sore throat, and the flu walk into a bar, the bartender says, "What is this, some kind of sick joke?"@@ A woman called her doctor and said, "I think I have the flu." The doctor said, "Well, take two aspirin and call me in the morning." The woman said, "I don't have two aspirin." The doctor said, "Well, take one and call me in the morning." The woman said, "I don't have one." The doctor said, "Well, just call me in the morning."@@ I once caught the flu... ...at the Airport. Think it was a Terminal Disease
Courtesy of:
John H. Keefe III, D.C.
CHIROPRACTIC MONTH: American Chiropractic Association (ACA) has announced a national health care observance--October is
National Chiropractic Month
DO YOU KNOW SOMEONE WITH A HEALTH PROBLEM OR IN PAIN? INVITE YOUR FAMILY OR FRIENDS TO THE PARTY
Who do you know who is hurting? Who do you know that you have been trying to get started at Keefe Clinic? Now is the time to get your spouse or child started on the road to good health.
Complimentary DIAGNOSTIC WORK UP DURING OCTOBER Complimentary initial exam and one X-ray. Tell someone today
IN THE NEWS: Two Types of People Who Should Never Get the Flu Shot Secondary infections such as pneumonia and other respiratory diseases, as well as sepsis, are included in “influenza death” statistics, and account for a majority of deaths attributed to influenza every year. U.S. Centers for Disease Control and Prevention data have repeatedly demonstrated that the flu vaccine does not work for seniors. The 2018/2019 flu vaccines against influenza A and B viruses had an adjusted effectiveness rating of just 12% for those over age 65. Studies have also demonstrated that influenza vaccination has little or no impact on mortality among the elderly. The flu vaccine is routinely recommended for all pregnant women during any trimester, yet some scientific evidence suggests it could place their pregnancy at risk. Research funded by the CDC found an association between flu vaccination during pregnancy and an eightfold risk of miscarriage. Injury following influenza vaccination is now the most compensated claim in the federal Vaccine Injury Compensation Program (VICP). Between January 1, 2006, and December 31, 2019, a total of 5,407 injury claims for flu vaccine were filed. Virulence January 1, 2014; 5(1): 137–142--Health October 2, 2018--Cochrane.org--Precisionvaccinations.com 2019-2020 Recommendations--CDC.gov Upcoming 2019/2020 Flu Season
WELLNESS: The vitamins in your foods are hard at work keeping you healthy. Vitamin A helps form and maintain healthy teeth, bones, soft tissue, mucous membranes, and skin. Vitamin B6 is also called pyridoxine. Vitamin B6 helps form red blood cells and maintain brain function. This vitamin also plays an important role in the proteins that are part of many chemical reactions in the body. The more protein you eat the more pyridoxine your body requires. Vitamin B12, like the other B vitamins, is important for metabolism. It also helps form red blood cells and maintain the central and peripheral nervous systems. Vitamin C, also called ascorbic acid, is an antioxidant that promotes healthy teeth and gums. It helps the body absorb iron and maintain healthy tissue. It is also essential for wound healing. Vitamin D is also known as the "sunshine vitamin," since it is made by the body after being in the sun. Ten to 15 minutes of sunshine 3 times a week is enough to produce the body's requirement of vitamin D for most people at most latitudes. People who do not live in sunny places may not make enough vitamin D. It is very hard to get enough vitamin D from food sources alone. Vitamin D helps the body absorb calcium. You need calcium for the normal development and maintenance of healthy teeth and bones. It also helps maintain proper blood levels of calcium and phosphorus. Vitamin E is an antioxidant also known as tocopherol. It helps the body form red blood cells and use vitamin K. Vitamin K is needed because without it blood would not coagulate normally. Some studies suggest that it is important for bone health. Biotin is essential for the metabolism of proteins and carbohydrates, and in the production of hormones and cholesterol. Niacin is a B vitamin that helps maintain healthy skin and nerves. It also has triglyceride-lowering effects at higher doses. Folate works with vitamin B12 to help form red blood cells. It is needed for the production of DNA, which controls tissue growth and cell function. Any woman who is pregnant should be sure to get enough folate. Low levels of folate are linked to birth defects such as spina bifida. Many foods are now fortified with folate in the form of folic acid. Pantothenic acid (vitamin B5) is essential for the metabolism of food. It also plays a role in the production of hormones and cholesterol. Riboflavin (vitamin B2) works with the other B vitamins. It is important for body growth and the production of red blood cells. Thiamine (vitamin B1) helps the body cells change carbohydrates into energy. Getting enough carbohydrates is very important during pregnancy and breastfeeding. It is also essential for heart function and healthy nerve cells. Choline helps in normal functioning of the brain and nervous system. Lack of choline can cause swelling in liver. Carnitine helps the body to change fatty acids into energy.
FUNNY BONE: What do dolphins need to stay healthy? Vitamin Sea! @@ I wonder if you can help me? I seem to be suffering from a lack of Vitamin U. @@ When life gives you lemons, make lemonade; when life gives you apples, make physics equations. (Looking at you Newton).
Visit our web sites:
keefeclinic.com & keefeclinic.quora.com
| Visit our web sites: keefeclinic.com & facebook.com/keefeclinic |

Pills, injections, and quick fixes might mask pain for a while, but they carry two serious dangers:
A Better Way: Natural Healthcare
Chiropractic, nutrition, and other natural healthcare approaches don’t chase symptoms. Instead, they look for the root cause. Misaligned joints, poor posture, inflammation, nutritional deficiencies, or lifestyle stressors — these are correctable. Once the cause is addressed, the pain doesn’t need to be “managed” because it resolves naturally.
The Choice Is Clear
You can cover up the pain and let the problem grow worse, or you can fix the problem and let the pain go away because the body has healed.
Natural healthcare isn’t about chasing symptoms. It’s about restoring balance, correcting causes, and giving the body what it needs to heal itself. Pain is a warning light — don’t put tape over the dashboard. Open the hood, fix the problem, and keep the engine running strong.
When most people think of immunity, they picture white blood cells fighting infection or maybe the lymph nodes swelling when the body is battling a virus. But there are two small, often-overlooked organs that play central roles in keeping the immune system strong: the spleen and the thymus.
The spleen acts as a kind of immune filter. It screens the blood for pathogens, removes damaged red blood cells, and produces immune cells (lymphocytes) that respond to infections. When the spleen is weakened or removed, people are more vulnerable to severe infections—especially from encapsulated bacteria like Streptococcus pneumoniae and Haemophilus influenzae .
The thymus is sometimes called the “training academy” for T-cells. Immature immune cells migrate there to learn how to recognize invaders while ignoring the body’s own tissues. If the thymus is underactive or absent, the immune system becomes confused and either fails to defend against infections or mistakenly attacks the body (autoimmune disease). Severe thymic defects are associated with conditions like DiGeorge syndrome (immune deficiency), while thymic abnormalities have been linked with autoimmune disorders such as myasthenia gravis .
While mainstream medicine has few tools to directly “strengthen” these organs, natural healthcare offers several supportive strategies:
A healthy immune system doesn’t just depend on “strong white cells.” It depends on a finely tuned system where the spleen filters and arms the blood, and the thymus trains the soldiers. Supporting these organs naturally—with nutrition, stress reduction, spinal care, and immune-strengthening herbs—can reduce the risk of both infections and autoimmune problems.
References

For centuries, mushrooms have been prized not only as food but as natural medicine. Modern research is confirming what traditional systems already knew: each mushroom species has a unique profile of compounds—beta-glucans, antioxidants, and other phytochemicals—that support different aspects of health. Here’s a guide to the most researched medical mushrooms, what they may help with, and how best to take them.
Mushrooms are not all alike. Some, like shiitake or maitake, can go straight into your stir-fry or salad bowl. Others, like reishi or turkey tail, are better taken in capsules or tea. Each has its own “specialty”—from brain health to immune support, from cholesterol to energy. Understanding their unique profiles allows you to use them wisely, whether in the kitchen or in supplement form.